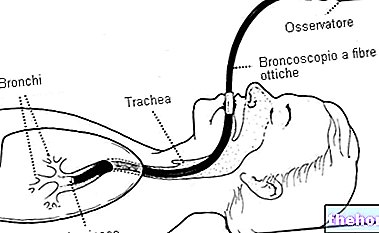
Also known by the abbreviation "Night Apnea", this problem is characterized by repeated episodes of obstruction of the upper airways during the inspiratory phase which manifests itself as a partial reduction in the flow of air (hypopnea) or a "complete respiratory interruption (apnea). for a period> 10 seconds). Obstructive sleep apneas compromise the quantity or quality of sleep and lead to a reduction in the concentration of oxygen in the blood, as well as a series of clinical disorders that derive from the recurrence of the phenomenon.
emits low-frequency electrical waves (brain waves are fast and irregular in wakefulness). Muscle tone has decreased, but involuntary motor activities are occasionally recorded (e.g. when changing position in bed). Even myocardial consumption of oxygen and blood pressure undergo a reduction, as well as the heartbeat slows down considering the prevalence of vagal tone: in practice, the non-REM phase coincides with a rest period for the cardiovascular system.
REM sleep follows each NREM sleep cycle and corresponds to approximately 20% of the total rest time (note: normally, sleep stages do not occur once a night, but alternate several times for a total of 5- 6 complete cycles lasting 90-100 minutes). The REM phase is characterized by high-frequency electroencephalographic waves and episodes of rapid eye movements below the closed eyelids. The postural muscles lose tone, however the muscles that control the face, eyes and distal leg frequently become phasic. Compared to slow wave sleep (NREM phase), in this period there is an increase in brain activity except in the limbic system, where, on the contrary, neuronal activity decreases. It is in this stage that the dream activity occurs: the dreams are more elaborate and intense and are generally very articulated.
What Happens in Obstructive Sleep Apnea Syndrome
In obstructive sleep apnea syndrome, abrupt "sympathetic-vagal" transitions occur in correspondence with the "apnea-awakening" events. These result in a fragmentation of sleep. In addition to the chronic snoring typical of obstructive sleep apnea, patients often present with daytime sleepiness, slowing of reflexes, reduced attention span, extreme fatigue and loss of all energy, depression or irritability and altered socio-family relationships. In addition, cardiovascular (acute and chronic) and cerebrovascular complications have been reported in patients with sleep apnea.
they are different and can occur during sleep, upon waking, or during the day.
The interruption of a person's regular breathing activity when sleeping is responsible for restless, poor quality and unrefreshing sleep, with both nocturnal and diurnal symptoms.
Obstructive sleep apnea: what are the main symptoms?
- During the night, sleep apnea involves sudden awakenings with a sense of suffocation and intense snoring, often interrupted by pauses of silence and labored breathing.
- During the day, symptoms are agitation, fatigue, difficulty concentrating, a feeling of not having rested well, decreased interest in sex, morning headache, and excessive daytime sleepiness.
Cardiovascular Effects of Obstructive Sleep Apnea
In the long term, sleep apnea is an "important cause or contributing cause of cardiovascular morbidity and mortality. In particular, obstructive sleep apnea syndrome can lead to the development of arterial hypertension, cardiovascular disease, respiratory failure and metabolic disorders.
and vessels as a mechanical and biohumoral insult.
In moderate and severe forms (AHI / Apnea-Hypopnea Index> 30 episodes of apnea and / or hypopnea per hour of sleep), the risk of fatal cardiovascular accidents is estimated to increase by about 4-5 times compared to that of healthy subjects.
In addition, patients with obstructive sleep apnea are twice as likely as healthy people to experience sudden death between midnight and six in the morning.
Hypertension
High blood pressure affects approximately 60% of patients with obstructive sleep apnea syndrome.
Apnea - understood as complete respiratory interruption for a period> 10 seconds - causes hypoxemia and represents a stimulus to the nocturnal secretion of catecholamines, with subsequent increase in peripheral resistance and blood pressure, up to hypertensive crisis and acute pulmonary edema.
Recurrent apneas and persistent catecholaminergic state favor the development of arterial hypertension ("non-dipper" model); for example, an apnea / hypopnea index (AHI) of 10 corresponds to a relative risk of developing arterial hypertension of 11%.
Diastolic dysfunction
Obstructive sleep apnea syndrome also correlates with an increased risk of developing ventricular hypertrophy (left and / or right).
Right ventricular hypertrophy can lead to right ventricular dilation due to:
- Vasoconstriction of pulmonary arterioles (increased afterload);
- Greater venous return to the right ventricle during apnea (increased preload).
Finally, ventricular hypertrophy and interstitial fibrosis can alter diastolic function; about 41% of patients with obstructive sleep apnea syndrome present impaired relaxation. In addition, in apnea, the intrathoracic pressure becomes more negative, the return venous to the right ventricle increases and the interventricular septum protrudes into the left ventricular cavity, reducing its filling.
Myocardial ischemia and atherosclerosis
Approximately 20% of patients with obstructive sleep apnea syndrome have nocturnal episodes of angina pectoris and / or silent ST segment elevation, resulting from tachyarrhythmias and the discrepancy between hypoxemia (caused by "apnea) and increased myocardial oxygen consumption for high peripheral arteriolar resistance.
On the other hand, obstructive sleep apnea syndrome is often associated with multiple coronary risk factors, which promote the progression and instability of atheroma, including:
- Diabetes mellitus;
- Dyslipidemia and visceral obesity;
- Smoke;
- Pro-inflammatory state (C-reactive protein, IL 6, TNF alpha, cell adhesion molecules)
- Endothelial dysfunction.
The reaction between obstructive sleep apnea syndrome and atherosclerotic risk is not of simple association, but of cause and effect; in fact, the fragmentation of sleep induces the secretion of inflammatory pro-inflammatory cytokines and metabolic disorders (production of leptin, hyperinsulinemia).
Arrhythmias
Obstructive sleep apnea syndrome may be a condition at risk of sudden arrhythmic death, favored by the high nocturnal variability of the R-R interval.
In apnea, vagal hypertonus predisposes to bradycardia and atrioventricular blocks, while subsequent sympathetic hypertonus facilitates the onset of:
- Paroxysmal atrial fibrillation;
- Ventricular extrasystole;
- Non-sustained ventricular tachycardias.
Recent preliminary studies suggest that the implantation of atrioventricular pacemaker prevents bradyarrhythmias, reduces the dispersion of the refractory period of the atrial and ventricular myocardium, preventing threatening tachyarrhythmias.
Heart failure
Almost half of chronic heart failure patients have obstructive sleep apnea syndrome.Obstructive Apnea is less frequent than Central Apnea, but mixed forms are not uncommon.
- Obstructive Apnea is more frequent in the obese, in whom the edema of the pharyngo-tonsillar structures favors the periodic narrowing of the upper airways.
- Central apnea is observed rather in patients with severe left ventricular dysfunction, NYHA 3-4 class, awaiting cardiac transplantation; these patients, basically hypoxemic and hypocapnic, after apnea have a more pronounced hypocapnia which inhibits the centers of the CNS breath, resulting in Cheyne Stokes' periodic breathing.
Some studies have shown that about 51% of patients with chronic systolic heart failure have an apnea / hypopnea index (AHI) greater than or equal to 15 (40% are Central Apneas and 11% Obstructive Apneas), while 50% of patients with diastolic heart failure have an apnea / hypopnea index (AHI) greater than or equal to 10.
Patients with chronic heart failure and Cheyne Stokes' periodic breathing have significantly reduced survival compared to other patients with chronic heart failure. Hypoxemia secondary to apnea stimulates the production of catecholamines, with the risk of acute pulmonary edema and tachyarrhythmias, which are extremely dangerous in patients who have a precarious cardiovascular compensation.
Other articles on "Obstructive Sleep Apnea Syndrome and Heart Disease"
- Obstructive Sleep Apnea Syndrome - Therapy
- Night Apnea: Also a Problem of Safe Driving
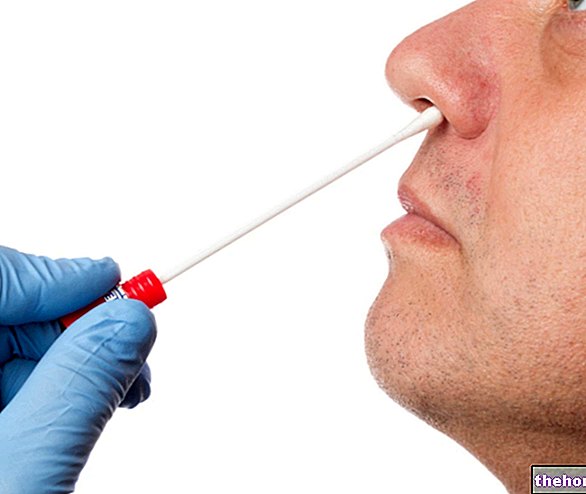
- Night Apnea and Safe Driving: Diagnosis Tests