Generality
Osteonecrosis means death of bone tissue.
Contrary to what many believe, bone is a living tissue, which needs blood and oxygen; if these are missing, the cells that compose it undergo premature death and osteonecrosis occurs.

Figure: X-ray of the shoulder joint; the image on the right shows the osteonecrosis process affecting the head of the humerus and the glenoid cavity of the scapula. From the site: www.drlox.com
It can lead to local fractures and, in the most severe cases, the collapse of the affected bone.
The factors that can trigger an osteonecrosis process are numerous, including joint trauma, abuse of corticosteroid drugs, alcoholism, sickle cell anemia, etc.
In general, the epiphyses of the long bones are mainly affected, ie the terminal tracts of bones such as the femur, tibia or humerus involved in the respective joints.
Pain and poor joint function are the main symptoms of osteonecrosis.
Therapy consists of various remedies, both conservative and surgical. To avoid complications, it is good to intervene promptly.
What is osteonecrosis?
Osteonecrosis is the death of bone tissue, due to a lack or insufficient blood supply. Also known as avascular necrosis, bone necrosis or bone infarction, it results in the appearance of tiny fractures in the affected bone tract; in the most cases severe, osteonecrosis can even lead to bone collapse.
EPIDEMIOLOGY
Osteonecrosis can affect anyone, however, according to some statistical surveys, it is more common among males between the ages of 30 and 60.
Causes
The blood supply to a certain portion of bone can be impaired by:
- An injury to the nearby joint. The joint injuries that most frequently result in bone necrosis are knee sprains, dislocations of the shoulder or hip, sprains of the ankle, etc.
- Radiotherapy treatment for cancer (radiotherapy). The ionizing radiations used for the treatment of tumors can have unpleasant side effects; these also include weakening of the bones and damage to the blood vessels that supply the bone tissue and keep it alive.
- Sickle cell anemia. In this disease, the red blood cells have a particular shape, which makes the flow of blood inside the smallest blood vessels abnormal. This results in poor blood circulation and a lack of nourishment of some tissues, including bone.
- The abuse of alcohol. In the blood vessels of those who drink a lot of alcohol, fatty deposits are created, which prevent the blood from flowing freely. In the long run, these deposits can completely occlude the caliber of the vessels and cause episodes of osteonecrosis .
- Prolonged and / or high doses of corticosteroid and bisphosphonate drugs. Corticosteroids are powerful anti-inflammatories, while bisphosphonates are medicines used in case of osteoporosis. The former, if taken in excessive doses, can cause various side effects, including accumulations of fat inside the vessels and their consequent occlusion (N.B: the process is very similar to what happens in the case of alcohol abuse).
The latter, on the other hand, if taken in high doses can cause a process of osteonecrosis of the jaw (N.B: the pathophysiological mechanism, for bisphosphonates, has not yet been fully clarified).
In addition, according to some studies, they are more at risk of osteonecrosis:
- People suffering from particular morbid conditions, such as diabetes, AIDS, systemic lupus erythematosus, the so-called decompression sickness, hypertension, Gaucher's disease, arterial thrombosis, arterial embolism and rheumatoid arthritis.
- People who have had an organ transplant or who are undergoing dialysis because of a severe kidney problem.
Finally, a small number of people with osteonecrosis develop the problem for no particular reason. In these situations, we speak of idiopathic osteonecrosis.
Symptoms and Complications
For further information: Osteonecrosis Symptoms
Very often, in the early stages, osteonecrosis turns out to be asymptomatic (ie it does not cause any obvious symptoms). Then, over time, it becomes the cause of unusual pain and fractures.
In the most severe stages (complications), the necrotic bone completely gives way (collapsing).
If the death of the bone tissue also involves a joint (very frequent), this can degenerate in a worrying way, even losing its functionality.

Figure: head of a normal femur (left) and affected by osteonecrosis (right). The blue capillaries indicate the avascular origin of the process; note also the rarefaction of the necrotic bone tissue. From the site: www.drlox.com
WHICH BONES ARE THE MOST AFFECTED?
The bones most affected by osteonecrosis are the long bones of the human body, such as the femur (ie the thigh bone) and the humerus (ie the arm bone).
This is true both when the causes are traumatic and when the patient abuses certain substances or is affected by one of the health disorders mentioned in the chapter dedicated to the causes.
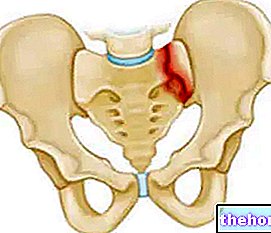
To fracture, and eventually to collapse, are the epiphyses, or the terminal portions of the long bones that participate in the joints.
WHICH JOINTS ARE THE MOST AFFECTED?
The joints most prone to osteonecrosis are the knees, shoulders, ankles, wrist, hip and jaw.
WHEN TO SEE THE DOCTOR?
It is advisable to contact your doctor when a certain bone or joint is strangely affected. If osteonecrosis is diagnosed in time, the most serious complications can be avoided.
Diagnosis
To diagnose osteonecrosis, a physical examination is not enough; many pathologies, in fact, have symptoms similar to those of a bone infarction. Hence the need to resort to specific instrumental tests.
The three most practiced tests are:
- X-ray examination. It is useful in detecting bone changes that occur in the advanced stages of osteonecrosis; in fact, at the outset, the problem is rarely identified.
During the radiographs the patient is exposed to a minimal dose of ionizing radiation. - Bone scan. Through the injection of a radiopharmaceutical intravenously, it allows to obtain images relating to the anatomy and activity of the bones. It is a very sensitive diagnostic test, because it clearly shows if there are any pathological changes; however, at the same time, it is a non-specific examination, as it does not clarify the nature of the disturbances highlighted.
The quantities of radioactive substance used are low, however bone scans are not recommended during pregnancy. -

Figure: the arrow indicates an "osteonecrosis of the femoral head. From the site: radiopaedia.org Nuclear magnetic resonance (NMR). It clearly shows the bone changes that occur in the advanced stages, while it is not always comprehensive in the early stages of the disorder.
A big advantage of MRI is that it is completely harmless to the patient.
THE PROBLEM OF LATE DIAGNOSIS
It often happens that osteonecrosis manifests itself with symptoms and signs only at an advanced stage, when the bone tissue is already partially compromised. In these cases, the diagnosis is inevitably late and this could affect the effectiveness of the treatments.
Treatment
To reduce the symptoms and slow down the progression of osteonecrosis, various drugs and some conservative treatments are available, such as simple rest and physiotherapy. However, when the bone infarction reaches a certain stage, these remedies may be ineffective or insufficient. On such occasions it is necessary to resort to more invasive treatments, of a surgical type, such as bone decompression or even the operation for the insertion of a joint prosthesis.
PHARMACOLOGICAL THERAPY
Possible medicines prescribed for cases of osteonecrosis are:
- NSAIDs, or Non-Steroidal Anti-Inflammatory Drugs. They are used to relieve the sense of pain and to reduce the inflammatory processes affecting the affected bone. The most used NSAID is ibuprofen.
- Some osteoporosis drugs. Research has shown that alendronate bisphosphonate, normally used for osteoporosis, also slows the progression of bone necrosis. However, it should be remembered that drugs belonging to the bisphosphonate class, if administered in excess, have several side effects, including osteonecrosis of the jaw.
- The cholesterol-lowering drugs. These medicines, by reducing the amount of lipids in the blood, are administered with the aim of improving blood circulation in the vessels that have caused osteonecrosis.
- Anticoagulants. They prevent the formation of blood clots and allow better blood circulation, even in the vessels involved in osteonecrosis.
REST AND PHYSIOTHERAPY
Rest is essential to avoid further stressing the suffering bone and / or joint. In cases of osteonecrosis involving the hip or knee, the use of crutches is recommended for a certain period of time.
Physiotherapy, on the other hand, is especially useful when the bone infarction has reduced the mobility of a joint.
SURGICAL THERAPY
Surgery is used when osteonecrosis is in very advanced stages, so it cannot be treated in any other way. Here are the surgical treatments available:
- Bone decompression. It consists in removing the diseased portion of bone, in order to stimulate the remaining healthy portion to regenerate new bone tissue.
- Bone transplant. It consists in replacing the diseased bone tract with a piece of bone taken from a healthy part of the body (autotransplant) or from a donor.
- Osteotomy. It consists in dissecting the diseased bone, removing some parts in order to redistribute, on a still healthy bone portion, the weight that weighs on the necrotic area. To be able to perform the osteotomy, obviously, the bone must still have areas of lively and strong tissue.
- Joint prosthesis. It is the intervention for the most serious cases, in which a bone collapse has occurred. There are interventions of hip prostheses, knee prostheses and so on.
Prevention
Preventing osteonecrosis due to certain health conditions is not easy at all.
However, it may be important to limit alcohol intake, keep blood cholesterol levels low and, if you are taking corticosteroids, strictly adhere to the doses recommended by your doctor.
Prognosis
Late therapy or lack of treatment make the prognosis negative, as osteonecrosis is a chronic-degenerative and debilitating problem.





















-nelle-carni-di-maiale.jpg)




