Septic arthritis: definition
In medicine, septic arthritis designates a complex clinical picture, supported by a "bacterial infection of a" joint: to create a similar damage, the pathogen, after invading the membrane and the synovial fluid, originates an exaggerated inflammatory response , which can lead to the formation of the so-called piartro, a purulent exudate in the joint space.
Generally, when treated early, septic arthritis responds well to antibiotic drug therapy; however, the morbidity and mortality of the disease should not be overlooked.

Incidence
Medical statistics show that septic arthritis occurs in 2-10 cases per 100,000 inhabitants annually; in the United States, for example, septic arthritis occurs in 7.8 per 100,000 healthy subjects. In Europe too, the data are similar. Putting more precise parameters, septic arthritis from streptococci seem to affect 2.6 people per 100,000, while disseminated gonococcal arthritis 2.8 subjects every 100,000.
An estimated 25-50% of patients suffer permanent damage, while 5-15% of the patients, not undergoing or not responding adequately to treatment, are destined to die.
Septic arthritis seems to be an increasingly imminent danger for the elderly, especially in conjunction with multiple diseases and immunosuppression.
An obstacle not to be overlooked is represented by the often very high costs for hospitalization of the patient, for the application of prostheses and for disability.
Causes
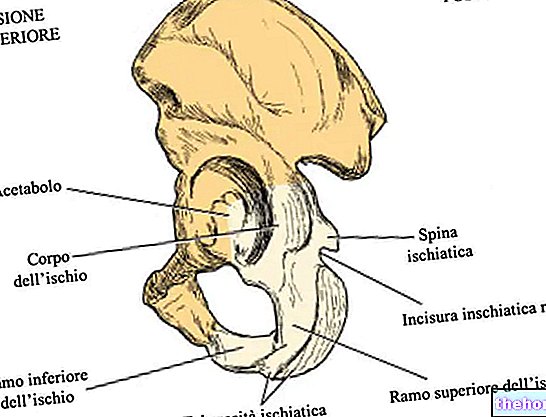
Although virtually any infectious agent can cause septic arthritis, in most cases, bacteria are the main culprits. The penetration of bacteria is favored both by the absence of the basement membrane and by the high vascularity of the synovium: the pathogens reach the site of action by haematogenic route. Although any joint can be affected by the infection, therefore developing septic arthritis, the The sites most involved are the hip, knee and shoulder.
It often happens that the pathogens, after reaching the blood, reach the joints and invade the synovial membrane; subsequently they are phagocytosed by the mediators of inflammation and by fibroblasts. The necrosis and swelling of the synovial membrane and of the cartilage that follow are an expression of the massive release of proteolytic enzymes and of the accumulation of purulent synovial fluid.
In some cases, septic arthritis constitutes a complication of arthroplasty (incidence index: 1-15%); in others, however, the infection occurs after the direct inoculation of pathogens (eg administration of drugs by intra-articular route, arthrocentesis, interventions on the joint).
How can septic arthritis arise?
- By direct inoculation, following intra-articular injections
- By the hematogenous route, typical of drug addicts, patients undergoing catheterization and suffering from endocarditis
- By hematogenous spread from a distant outbreak (similar to "osteomyelitis)
Risk factors
Some subjects are more at risk of septic arthritis, probably due to old age or the co-presence of degenerative diseases. The most common predisposing factors are summarized below:
- AIDS
- Arthrosis
- Catheterization
- Systemic connectivitis: rheumatoid arthritis, systemic lupus erythematosus, gout
- Haemophilia
- Diabetes mellitus
- Bacterial endocarditis
- Infant age (less than 3 years old) or advanced (over 80 years old)
- Prosthesis implant
- Long-term administration of steroids and immunosuppressants
- Drug addiction: mixed use of non-sterile syringes can promote infection
Resistance to antibiotics is also a real and particularly felt problem: some pathogens seem to resist even heavy antibiotic therapy.
Microorganisms involved
The vast majority of septic arthritis is triggered by infections caused by the Staphylococcus aureus; however, streptococci are also often involved etiopathological elements. The gonococcus (Nesseria gonorrhoeae) is the pathogen that is most often responsible for septic arthritis in sexually active adults. The bacterium Haemophilus influenzae on the other hand, it seems to be the gram-negative bacterium responsible for most of the acute septic arthritis in children (2-3 years).
Rarer, though possible, HIV-mediated septic arthritis, from Mycobacterium tuberculosis (carries tuberculosis), Borrelia burgdorferi (protagonist of Lyme disease), Group A beta-hemolytic streptococcus, Pseudomonas aeruginosa, Aspergillus spp. And Candida spp..
Clearly, vaccination (when possible) is an "excellent defense weapon to protect against infections in general and septic arthritis in particular."
The table shows the pathogens most involved in the various forms of septic arthritis.
Type of septic arthritis
Microorganism involved
Non-gonococcal septic arthritis
Staphylococcus aureus (> 70%), Group B, C, G hemolytic streptococci, Streptococcus pneumoniae, Borrelia burgdorferi, Brucella burgdorferi
Gonococcal septic arthritis
Neisseria gonorrhoeae (
Viral septic arthritis
HBV, HIV 1, Rubella, Parvovirus B19
Septic mycobacterial arthritis
M. tuberculosis
Fungal septic arthritis
C. albicans, S. schenckii, C. immitis
Postinfectious septic arthritis
Shigella spp, Campylobacter spp, Salmonella spp, Yersinia spp, Chlamydia spp.
Other articles on "Septic Arthritis"
- Septic Arthritis - Symptoms, Diagnosis, Treatment
- Septic Arthritis - Drugs to Treat Septic Arthritis