What is the Amniocentesis?
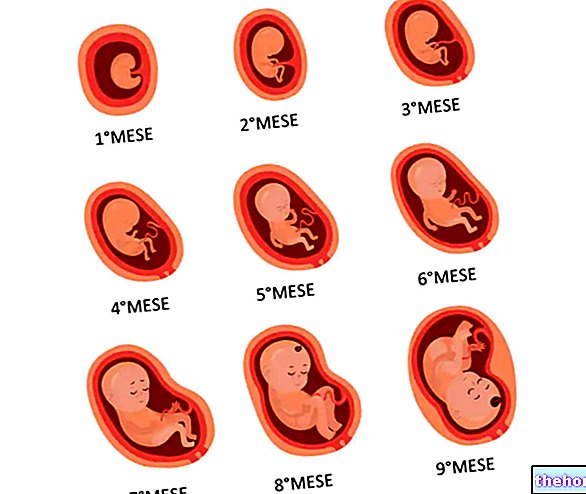
Amniocentesis consists in the transabdominal removal of a small amount of the amniotic fluid, which envelops and protects the fetus during its growth and development.
In the womb, the fetus is housed inside a sac, called the amniotic sac or amnios, filled with a fluid - the amniotic fluid - which protects it from shocks, temperature changes and pressures of various kinds.
Why is it done?

Index Insights
Technique and risks
As a rule, amniocentesis is performed starting from the fifteenth week of pregnancy, when the amniotic cavity has reached such dimensions that it does not pose particular risks to the fetus during the examination. These risks are further reduced by a preventive ultrasound, which shows the position of the fetus and placenta. If the pregnant woman is suitable for the examination - which, for example, is contraindicated in the presence of fever or other current infections - the skin of the abdomen is disinfected with an antiseptic solution. Under constant ultrasound guidance, the obstetrics and gynecology specialist inserts a very thin needle through the skin that covers the underlying uterine cavity, in order to reach the amniotic cavity and withdraw about 15 ml of the liquid of the same name. Consider that at the 14th week of gestation this liquid occupies a volume of about 100 ml, which rises to 150-200 ml 15/30 days later and to 500 ml around the twentieth week. Ultrasound monitoring does not produce ionizing radiation, is absolutely harmless and as such does not cause any damage to the indeed, it allows to control its position and that of the needle, minimizing the risk of complications.
In the laboratory, a small part of amniotic fluid is used to perform direct biochemical tests, while the remaining fetal cells are isolated, subsequently cultured to obtain a numerical sample sufficient for the evaluation of the karyotype.
The examination is not painful (at most annoying), lasts a few minutes and does not require special anesthesia or hospitalization; at the end of the amniocentesis it is still necessary to stay in the health center for 30-60 minutes. In the 2/3 days following the examination it is advisable to refrain from heavy physical activities; moreover, in case you experience prolonged abdominal pain or the appearance of fever or strange vaginal discharge, it is important to immediately inform your health care assistants.
Like all invasive procedures, even if practiced by experienced and well-equipped personnel, amniocentesis presents a certain percentage of abortion risk, roughly quantifiable in one possibility in 200. More recent studies, dated 2006, indicate that the additional risk of abortion, compared to women not subjected to amniocentesis, it is particularly low (0.06%) if not even zero. It is therefore a safe procedure, characterized by a very small percentage of risks and complications. One of these is canceled by administering Rh negative pregnant women non-immunized, with Rh positive partner, anti-D immunoglobulins; the injection of these antibodies is necessary for the possible passage of fetal blood into the maternal circulation, with consequent production of immunoglobulins that could harm the baby.
Theoretically, abortion associated with amniocentesis can be traced back to the development of amniotitis (infection of the amniotic fluid), rupture of membranes or the appearance of contractile activity that cannot be controlled with medical therapy. Diagnostic errors and culture failures that require repetition of the test are extremely rare (<0.2%). Because of these risks it is absolutely necessary that the amniocentesis be preceded by the signing of the informed consent by the pregnant woman, who has the right to obtain in advance all kinds of explanations on modalities, limits diagnostics and risks of the procedure.
Considering the costs and above all the rare, but still possible, complications, amniocentesis is not carried out if the parents exclude a priori any hypothesis of pregnancy termination, unless they want to perform it for the sole purpose of preparing with greater awareness at the birth of a child affected by some anomaly. Furthermore, it is not a routine examination, but a "diagnostic investigation to which only consenting mothers considered at risk are subjected. Beyond this, amniocentesis is still an absolutely optional examination and the parents are solely responsible for their choice.
Other articles on "Amniocentesi"
- Amniotic fluid
- Amniocentesis: to perform it or not to perform it














.jpg)











