These absorption capacities are not even constant over the course of life: the amount of calcium absorbed remains around 75% up to the age of 20, drops to 40% in adults and 20% in the elderly. However, in the first year of life the daily requirement is 500mg, from 1 to 6 years of 800mg / day, from 7 to 10 years of 1000mg, from 11 to 19 years of 1200mg, from 20 to 29 years of 1000mg, in adulthood of 800mg; after 60 years some recommend increasing the intake up to 1200 mg.
Pregnancy and breastfeeding require a surplus of 400 mg, determined not only by the increased losses, but also by the low level of estrogen.
The requirement of phosphorus is equivalent in grams to that of calcium; larger quantities in the adult do not create problems.
For further information: Calcium and Phosphorus , insufficient intake resulting from strictly vegetarian diets, intestinal diseases such as celiac disease, Crohn's disease, resections, severe renal dysfunction, estrogen deficiency and hypoparathyroidism. The first symptoms are a stinging sensation and paresthesia; the most characteristic symptom is tetany, up to convulsions in the most severe cases. In the child rickets and teething defects are found, in the adult osteomalacia.
The deficiency of phosphorus is very rare and usually consequent to the use of antacids that sequester it, preventing its absorption; other cases of deficiency have been found in the case of re-feeding of malnourished patients, if adequate phosphorus supplements are not administered (refeeding syndrome). Symptoms appear when plasma levels drop below 1 mg / l and are due to the reduced synthesis of high-energy compounds: it includes asthenia, muscle weakness, anorexia and general malaise; if the condition persists, osteomalacia may appear.
, given that healthy subjects tolerate quantities up to 2.5 g without any consequence; greater supplies hinder the absorption of iron. Hypercalcemia can be found in subjects with peptic ulcer who take large quantities of milk and alcohol or in individuals with severe renal insufficiency: in such cases there may be nephrocalcinosis, extrarenal calcinosis, alkalosis, hyperphosphorus, as well as reduced absorption of iron and other minerals.
Dietary excesses of phosphorus are very rare and linked to the massive introduction of aluminum phosphate-based laxatives.
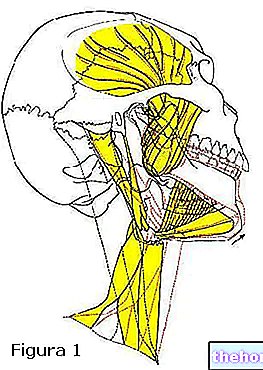
stimulates the production of parathyroid hormone by the parathyroid glands. This hormone acts in various ways:- Increases the reabsorption of calcium in the renal tubules;
- Increases bone resorption;
- Activates the renal enzyme that hydroxylates in position 1, activating it, vitamin D.
In turn, vitamin D acts at all three levels, kidney, intestine and bone, to restore calcium to its normal values.
The phenomenon of intestinal absorption deserves particular mention. It occurs in two ways: transcellular and paracellular.
In the first case, calcium passes through a channel of the apical membrane of the enterocyte, binds to CaBP, passes through the cytoplasm and is poured into the interstitial fluid by special pumps; vitamin D intervenes in this process by favoring the synthesis of pumps and CaBP, which by binding calcium, it not only allows it to pass through the cytoplasm, but prevents it from forming aggregates that block its channel.
Vitamin D also affects the second type of transport, modifying particular sites of the junctions and allowing an easier flow of the ion; however this mechanism is effective only at high intraluminal concentrations, also because the flow is allowed in both directions.
If, on the other hand, hypercalcemia occurs, the body reacts by blocking the synthesis of parathyroid hormone and vitamin D; calcitonin, produced by thyroid C cells, has an antagonistic effect of parathyroid hormone only at pharmacological concentrations.
Other hormones involved in calcium metabolism are:
- Glucocorticoids which lead to bone loss and reduced intestinal absorption;
- The growth hormone that stimulates the formation of cartilage and bone;
- Thyroid hormones that stimulate bone resorption;
- The lack of estrogen which promotes osteoporosis.
Phosphatemia, on the other hand, is kept constant with the regulation of excretion which is affected by dietary intake and absorption; it also increases in hyperparathyroidism, acidosis and following the use of diuretics; increased excretion is also found in prolonged fasting , caused by tissue degradation. Excretion, on the other hand, decreases in hypokalaemia in metabolic or respiratory alkalosis or due to increased plasma levels of insulin, glucagon, thyroid hormone, growth hormone. Even its absorption, like that of calcium, occurs according to two components, one passive and the other mediated carrier, and is affected by the presence of vitamin D.
The excretion in the form of urine varies between 100 and 350 mg per day. It increases with the increase of dietary proteins; however often a diet rich in proteins also provides phosphorus which counteracts this effect by stimulating the production of parathyroid hormone.