The term dyspepsia is of Greek origin (dys-pepto) and means "difficult digestion".

There are various forms of dyspepsia, which can be differentiated according to the predominant symptoms and the triggering cause.
The symptomatological picture can be variable, but it is always characterized by a feeling of digestive difficulty.
The causes are to be found in:
- Altered gastric adaptation to food intake.
- Delayed gastric emptying.
- Visceral hypersensitivity.
- Impaired motility of the small intestine.
- Alteration of motor nervous control.
What to do
- Identify the main symptoms, which must have been present for at least 6 months and consistently for the last 3:
- Epigastric pain.
- Postprandial fullness.
- Early satiety.
- Nausea.
- He retched.
- Belching.
- Contact your primary care physician or gastroenterologist, who will make the specific diagnosis.
- Based on the symptomatological picture, dyspepsia can be defined:
- Postprandial.
- Painful epigastric.
- Depending on the causes, however, dyspepsia can be defined:
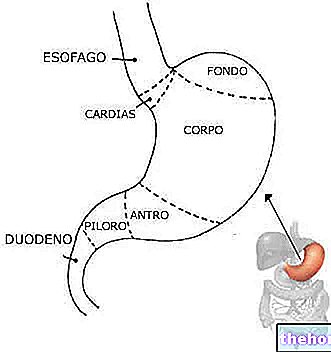
- Organic dyspepsia: secondary to pathologies of the digestive or extra digestive tract. The triggers can be different:
- Digestive disorders:
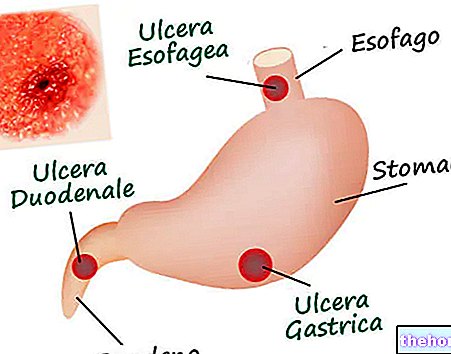
- Gastroesophageal reflux disease (GERD): the remedy consists of a specific diet, associated with lifestyle modifications. In addition, certain medications are recommended.
- Esophageal neoplasms: surgery is required.
- Peptic ulcer: Dietary therapy, lifestyle change, drug administration, and sometimes surgery is required.
- Gastric neoplasms: Surgery is required.
- Biliary lithiasis: a dedicated diet, drug administration and sometimes surgery is required.
- Pancreatopathies: the remedy varies according to the etiological agent.
- Extradigestive pathologies (we will not mention the specific remedy as it is beyond the scope of the article):
- Endocrinopathies.
- Congestive heart failure.
- Kidney failure.
- Collagenopathies.
- Vasculitis.
- Digestive disorders:
- Functional dyspepsia: recognizable by the absence of organic problems (digestive or systemic). The cause could be a motor dysfunction caused by the loss of nitrergic neurons in the stomach wall (sensory and motor).
- Organic dyspepsia: secondary to pathologies of the digestive or extra digestive tract. The triggers can be different:
NB: Organic dyspepsia has a "high percentage of comorbidity" for Helicobacter pylori infection. However, there is no scientific evidence that the latter can alone be responsible for dyspepsia.
What NOT to do
- Ignore the symptoms: since dyspepsia can be caused by even serious diseases, ignoring the symptoms can lead to a deterioration in health.
- Do not seek medical attention.
- Eating a diet and lifestyle that worsens digestion and symptoms.
- After diagnosis, do not comply with specific therapy.
What to eat
Diet for dyspepsia is a very important factor, but general advice is not very specific; in case of comorbidity it is necessary to respect the precise rules of the pathology:
- Chew thoroughly.
- Do not drink excessively during meals and do not eat "dry": 1-2 glasses per meal are enough.
- Regularize meals.
- Divide the diet into at least 5-6 meals a day, of which the most abundant must be lunch. For example: 15% of calories at breakfast, 3 snacks at 10%, lunch 30% and dinner at 25%.
- Share calories in a balanced way; the ration of fats assumes particular importance, which should be consumed in proportions equal to 25% of the calories consumed. It is sufficient to consume partially or totally skimmed milk / yogurt, very few cheeses, lean meats and fish, a couple of whole eggs a week, no more than 10g of dried fruit a day and season each dish with only 1 teaspoon of oil.
- Choose portions and meals of appropriate size: for example, no more than 80g of pasta or dried legumes, no more than two slices of bread per meal, no more than 150g of meat or fish, no more than two eggs at a time (cooked without fats) etc.
- Except for nighttime sleep, allow no more than 3 hours to pass between meals.
- Prefer light cooking methods: boiling, steaming, sous-vide, pot cooking, etc.
What NOT to Eat
- Avoid large meals.
- Avoid large portions.
- Avoid fasting.
- Avoid eating before bed or overeating before staying still (lying down or sitting).
- Many dyspepsia diagnoses are complicated by a "food intolerance or" allergy. The first rule is to eliminate all the factors responsible for adverse reactions; the most frequent are lactose (lactose intolerance) and gluten (celiac disease).
- Especially in painful ulcer-like dyspepsia, it is necessary to eliminate:
- Irritating foods: chili, pepper, excess garlic and onion, ginger, horseradish, wasabi etc.
- Excess alcohol.
- Beverages and foods containing xanthines: coffee, tea (especially fermented), cocoa, chocolate, energy drinks, etc.
- Acidic and / or carbonated drinks: cola, carbonated, orange soda etc.
- Especially in dyspepsia with dysmobility and postprandial sense of fullness, it is necessary to eliminate:
- Excessive seasonings, especially of poor nutritional value: margarine, palm or plamistus oil, other hydrogenated or bi-fractionated vegetable oils, lard, dripping fat, etc.
- Fatty foods, especially of low nutritional value: mascarpone, cream, cold cuts, fast food meat, fried foods, snacks, sweets, etc.
- Avoid foods that negatively affect the trophism of the lower esophageal sphincter: for example, mint, cocoa, etc.
- Avoid heavy cooking methods: frying, stewing etc.
Natural Cures and Remedies
Like other therapies, they are extremely specific. Below we will list the most used ones:
- For dyspepsia caused by gastroesophageal reflux disease:
- Alkaloids with anticholinergic action that reduce gastric secretion:
- Atropine and scopolamine: contained in the leaves of Atropa belladonna. ATTENTION! Its use is no longer recommended due to potential side effects; moreover, the berries of the same plant are highly poisonous.
- Mucilaginous drugs that protect the mucous membrane of the stomach and esophagus:
- Marshmallow, alginic acid, mallow, Icelandic lichen and aloe gel.
- For dyspepsia caused by gastritis and peptic ulcer:
- Sodium bicarbonate (NaHCO3): in aqueous solution, it intervenes quickly, but causes some side effects such as: alkalinization of the urine, swelling, hypersodemia and sometimes diarrhea.
- Herbal medicine: some plants are able to improve the symptoms of peptic ulcer or to act positively on the mechanism of action. The best known are:
- Hypericum.
- Licorice.
- Passionflower.
- Chamomile.
- Consolidate.
- Calendula.
- Alginates and mucilaginous drugs that cover the gastric mucosa, protecting it from aggressive agents:
- Melissa.
- Altea.
- Mauve.
- Icelandic lichen.
- Calendula.
- Healing effect mother tinctures:
- Salicaria
- Strawberry.
- Garlic: can facilitate the eradication of Helicobacter pylori, but it stimulates gastric secretion and is contraindicated for ulcer (see Helicobacter pylori - Defeat it with Natural Remedies.
- Clove essential oil.
- For dyspepsia caused by biliary lithiasis disease:
- Milk thistle.
- Artichoke.
- Elecampane.
- Fennel.
- Aubergine.
- Borage.
- Peppermint.
- Absinthe.
- Oats.
- Cherry.
- Onion.
- Strawberry.
- Lemon.
- Grape.
- Rhubarb.
- Boldo.
- Aloe.
- Chicory.
- Rosemary.
- Dandelion (controversial).
Pharmacological treatment
- For dyspepsia caused by gastroesophageal reflux disease and peptic ulcer:
- Antagonists of histamine H2 receptors: ranitidine, cimetidine (eg Ulis, Biomag, Tagamet), famotidine and nizatidine (eg Nizax, Cronizat, Zanizal). For oral use and rarely parenteral, they inactivate the proton pump and reduce the release of hydrogen ions.
- Antacids (such as aluminum hydroxide with magnesium hydroxide, for example Maalox plus).
- Proton pump inhibitors: block the production of histamine, gastrin and acetyl choline; in association with antibiotics, they favor the elimination of Helicobacter pylori. Eg:
- Pantoprazole (such as Peptazol, Pantorc, Nolpaza, Gastroloc).
- Omeprazole (such as Antra, Nansem, Losec, Xantrazol).
- Lansoprazole (such as Pergastid, Lomevel, Lansox).
- Protectors of the gastric mucosa:
- Sucralfate (e.g. Degastril, Citogel).
- Compounds of bismuth (e.g. bismuth salicylate).
- Prostaglandin analogues: protect the mucosa by reducing gastric secretion; eg Misoprostol (such as Cytotec).
- Antibiotics against Helicobacter pylori:
- Amoxicillin: for example Augmentin, Klavux.
- Metronidazole: for example Metronid, Deflamon.
- Clarithromycin.
- For dyspepsia caused by biliary lithiasis:
- Ursodeoxycholic acid or ursodiol (eg Ursobil HT, Ursodes AGE Acid, Litursol): they tend to dissolve small and transparent stones.
- Terpenes: make bile more soluble.
- Chenodeoxycholic acid: tends to dissolve stones.
- Thiazide diuretics (eg. Hydrochlorothiazide: eg. Moduretic, Esidrex): useful against calcium aggregations.
Prevention
The prevention of dyspepsia, whenever possible, could be summarized as follows:
- Preventing or treating gastroesophageal reflux disease.
- Helps to avoid the onset of esophageal neoplasms.
- Prevent or cure gastritis and peptic ulcer.
- It helps to avoid the onset of gastric neoplasms.
- Prevent or cure biliary lithiasis.
- Preventing or treating pancreatopathies.
- Avoid the loss of gastric neurons: it is typical of severe gastric pathologies.
Medical Treatments
- In the case of cancer, surgery is aimed at removing the latter and the compromised tissues.
- For dyspepsia caused by gastroesophageal reflux disease:
- This operation can be performed in laparoscopy (fundoplication), with the aim of restoring the functionality of the gastroesophageal sphincter.
- For dyspepsia caused by peptic ulcer:
- Excision of the gastric branches of the vagus nerve, with the aim of reducing gastric secretion.
- Gastrectomy: resection of a part of the stomach.
- For dyspepsia caused by biliary lithiasis:
- Traditional cholecystectomy: invasive; it involves a major surgical cut but has a very high success rate.
- Videolaparosurgery: minimally invasive; the cuts are small but it is limited when the gallbladder is hidden. In this case, the traditional method is used.













.jpg)