The human being is constantly exposed to fungi. Most people tolerate this exposure without consequences. There are at least two reasons that explain this phenomenon: first, immunocompetent subjects (that is, with a normally functioning immune system), have a high level of innate resistance to fungal colonization; second, most fungi have low intrinsic virulence (they are poorly aggressive).
However, under conditions that lead to the debilitation of the host, many individuals become susceptible to fungi, Candida including.
If the diagnosis is late and the treatment is not aggressive, and if management of the underlying conditions that cause the host's debilitation is neglected, the fungal infection can become fatal.
Once considered rare and exotic, these infections have now become more common and medically important. This is due to the acquired immunodeficiency syndrome (AIDS), the increased use of radiotherapy and chemotherapy for the treatment of patients with malignant tumors and for the use of drugs suppressing the immune system (immunosuppressants) in the prevention of rejection after transplantation. "organ.
Since these mushrooms (including Candida) become pathogenic when the host is in a debilitated condition, experts commonly define them as opportunistic fungi.
in many areas of the human organism in the form of yeast (a microorganism formed by a "single cell).
By commensal we mean an organism (in this case the mushroom) that lives in close relationship with another organism (the human body) and that benefits from it without the human body itself having neither benefits nor disadvantages.
If it is not pathogenic, Candida it is always in the form of yeast, both at 37 ° C, which is the temperature of the human body, both at room temperature.
When it becomes pathogenic, it emits protrusions from its membrane and becomes a "hypha (that is, it has branches or filaments that stretch to their apex); in this state, it has the ability to" hang "on the underlying tissues and become an opportunist , that is, it takes advantage of a situation of immunosuppression to proliferate in an exaggerated way and cause the candidiasis disease (or candidiasis).
When Candida cause candidiasis is to all intents and purposes also a parasite, that is an organism that lives on or inside a host and from which it benefits without giving any useful contribution in return, or even causing damage to the host.
In some internal organs, always as an opportunist, Candida it can also anchor itself in the form of mycelium (ie a set of hyphae), which is synonymous with mold.
human (mycosis = fungal infection) and constitutes one of the most important problems of the immunocompromised subject (i.e. with an inefficient immune system).
Clinically, Candida it can cause superficial infections of the skin and mucous membranes, deep infections and generalized infections (more correctly we speak of systemic infections).
The genre Candida it includes about 150 species, of which about ten are potentially pathogenic to humans.
Among the pathogenic species, the main one is Candida albicans, but they also deserve a mention Candida tropicalis, Candida Krusei, Candida guilliermondi, Candida parapsilosis, Candida stellatoidea And Candida glabrata.
The aforementioned species, in particular Candida albicans, are part of the normal microbial flora of the human being and are found on the healthy mucous surfaces of the oral cavity, vagina, gastrointestinal tract and rectal area (up to 80% of the population has colonies of Candida in these offices, without being affected in any way).
On the contrary, the microorganism is rare on the skin of a healthy subject, with the exception of anatomical areas such as the armpit and the groin, in which the juxtaposition of two distinct skin areas creates a moist environment ideal for the growth of Candida.
If the human being is healthy, the Candida colonies present in the mucous membranes and on the skin are harmless, as the so-called good bacteria of the microflora and the immune system prevent their pathological proliferation.
However, when these two control systems fail, Candida begins to multiply intensively, triggering the condition known as candidiasis.
on the tongue, tonsils and soft palate; another example is vaginal candidiasis (or vaginal candida), which is typically responsible for pain and itching in the vulva.
Definitely rarer, but much more fearful, are systemic infections, which mostly affect immunosuppressed individuals, causing important complications, such as lung abscesses, endocarditis or meningitis; the leading example of systemic infection with Candida is the so-called invasive candidiasis (or invasive candida).
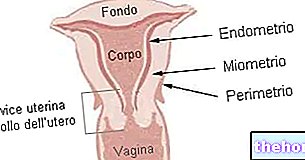
Vaginal candidiasis
Vaginal candidiasis (or vaginal candida) is a very common problem, especially among the female population of childbearing age. It is estimated, in fact, that about 75% of women experience this disorder at least once in their life; of these, about 4-5% will develop a recurrent form of infection, ie they will experience at least 3 episodes of acute vaginal candidiasis in a year.
The main culprit in vaginal candidiasis is Candida albicans; however, it should be noted that episodes of vaginal candidiasis sustained by other species of Candida less common and that mixed-type infections are also on the rise, ie due to both fungi and bacteria.
Being a widespread condition, vaginal candidiasis arouses considerable interest among the female population, therefore it deserves a special attention.
Finally, it should be noted that, when it concerns a full-term pregnant woman, vaginal candida represents a potential cause of oral candidiasis in the newborn.
Remember that ...
Candida albicans it lives normally with the organism, without creating particular problems. However, in the presence of some favorable situations it can grow quickly and abundantly, becoming aggressive and causing very annoying symptoms.
Oral Candidiasis
Oral candidiasis is the fungal infection resulting from the uncontrolled proliferation of the fungus in the mucous membrane of the mouth and throat Candida.
As with vaginal candidiasis, the species of Candida more often in oral candida is Candida albicans.
Thrush represents the most common form of candidiasis, the most widespread mycosis of the mouth and mycosis and the most recurrent opportunistic infection in humans.
Invasive Candida
Invasive candida is the infection resulting from the fungus passing through the blood Candida (fungemia or funghemia) and its spread to important organs, such as the heart (endocarditis), the brain (encephalitis), the eyes (endophthalmitis) or the bones (osteomyelitis).
Invasive candida can be fatal for the patient, therefore it represents a "medical emergency, which needs immediate help.
) and / or by circumstances that compromise the bacterial microflora responsible for controlling the growth of potentially pathogenic microorganisms (including Candida) present on the human body.
In the first case (immunosuppressive candida), the most common causative factors:
- Treatments with immunosuppressive drugs (used, for example, to avoid rejection in transplant patients or to control an autoimmune disease);
- Therapies based on chemotherapy (drugs typically used in the treatment of cancer), corticosteroids (particularly those inhaled) or disease-modifying antirheumatics (DMARDs);
- Radiotherapy (cancer treatment);
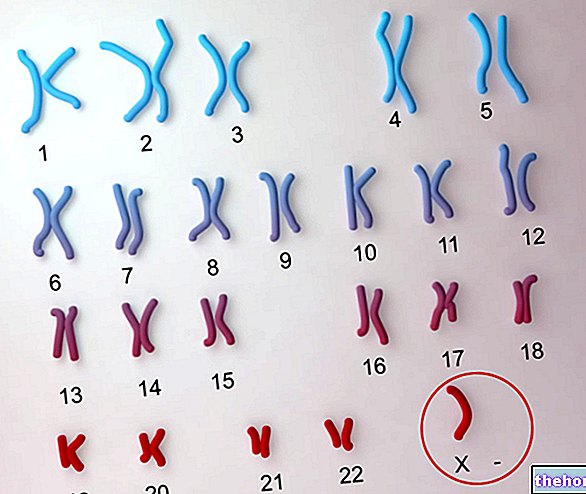
- AIDS, ie infection caused by HIV (human immunodeficiency virus);
- Some autoimmune diseases, including for example systemic lupus erythematosus, rheumatoid arthritis and Sjögren's syndrome;
- Diabetes mellitus;
- Vitamin and mineral deficiencies (deficiencies in iron, folic acid or vitamin B12 are important, for example);
- The burns;
- Psycho-physical stress.
In the second case (candida from compromised bacterial microflora), the typical cause is the long-term use of antibiotics, in particular those with a broad spectrum; for vaginal candida, moreover, the excessive use of detergents should also be reported intimate may play a key role in the "onset" of the infection.
Candidiasis: Risk Factors
The aforementioned conditions and behaviors certainly constitute a risk factor for candidiasis (therefore, inappropriate use of antibiotics or intimate cleansers; intake of chemotherapy drugs, immunosuppressants, inhaled corticosteroids, etc.).
To these, then, it is necessary to add:
- Excessive consumption of sweet foods (Candida it is a yeast whose growth and replication is favored by the presence of sugars such as sucrose);
- Sexual activity with infected people (this risk mainly concerns the man);
- The use of the estrogen-progestogen birth control pill, estrogen-based hormone therapies and pregnancy. It seems that the high levels of estrogen promote the growth and replication of Candida.
How Do You Get Vaginal Candida?
Vaginal candida can be transmitted through sexual intercourse and the shared use of towels or linen used by an infected person.
However, it is necessary to underline that the transmission of vaginal candidiasis by sexual route, unlike other infections of the vagina, is not very significant; more often, in fact, the vulnerability to this mycosis is due to stress, diabetes, prolonged use of antibiotics or corticosteroids and to imbalances in the normal vaginal or intestinal bacterial flora.
In general, all situations or diseases that weaken the body or lower the immune defenses can predispose to candidiasis, whether it is vaginal or elsewhere.
Vaginal Candida: what can alter the vaginal bacterial flora?
Especially in fertile women, the vagina hosts a microbial flora, rich in "good" microorganisms called lactobacilli, which protects it from infections, including those sustained by Candida.
However, when this microbial flora is exposed to factors such as the use of aggressive detergents or underwear that are too tight or nylon, its integrity and balance within it are undermined, which leads to a reduction in protection. guaranteed to the vagina.
It should be noted that, in a fertile woman, the microbial flora that protects the vagina from infections Candida it can also be affected by the use of oral contraceptives, hormonal changes in estrogen that occur during the menstrual cycle and pregnancy.
Oral Candidiasis: Causes
In addition to the factors listed above, the improper use of dental prostheses can also contribute to the development of oral candidiasis.
To prevent dentures from causing oral candida, it is essential to clean them properly and not use them overnight.
Systemic infections from Candida, on the other hand, they are spread to several organs (the term "systemic" means precisely this) and undermine their state of health as well as their function; a "systemic infection with Candida it can affect the brain, lungs, liver, eyes and bones at the same time, causing encephalitis, meningitis, pneumonia, hepatitis, endophthalmitis or osteomyelitis.
How Vaginal Candidiasis manifests itself: the Symptoms
In women, acute vaginal candidiasis is manifested by intense itching in the genital mucosa associated with the loss of whitish vaginal secretions; these losses, more or less abundant, frequently take on a dense and creamy appearance, similar to ricotta or curdled milk.
Alongside these typical symptoms, local irritation and swelling are often associated, burning during urination and pain in the vulva and vagina, even during sexual intercourse; precisely in reference to the latter, which in any case are often impractical because of the associated annoyance, the infectious agent Candida it can also infect the male genitals, causing some irritation, with redness, itching or burning of the glans (male candida or male candida).
Vaginal Candida: when to see a doctor?
In the presence of symptoms suggestive of a "vaginal infection from Candida it is advisable to contact your doctor or trusted gynecologist; the latter, once the symptoms and signs of the disease have been evaluated, will prescribe a vaginal swab: with the laboratory analyzes that follow the collection of the biological sample from the vagina, in fact, it is possible to isolate the infectious agent responsible for the condition in progress.
In particular, after the laboratory analysis, Candida it occurs in rounded, white or cream colonies.
Did you know that ...
In the "man, the search for a" genital infection from Candida occurs through a urethral swab.
(or antifungals).
Among the drugs used for the treatment of infections from Candida, stand out:
- Fluconazole, itraconazole and voriconazole, belonging to the pharmacological category of triazoles;
- Clotrimazole, econazole, fenticonazole nitrate, miconazole and ketoconazole, belonging to the pharmacological category of imidazole derivatives;
- Amphotericin B and nystatin, which, despite being part of the antibiotic category of polyene macrolides, have no antibacterial but antifungal power.
- Caspofungin, an antifungal from the category of echinocandins, used only in the most severe cases of candida.
The method of administration of these drugs varies according to the type of candidiasis and the severity of the infection, and can be oral (capsules or tablets), topical (cream or ovules) or intravenous.
For infections with Candida local, topical administration is often sufficient, although sometimes it may be necessary to use medicines for oral use; for infections caused by Candida of the systemic type, on the other hand, intravenous administration is essential.
It is important to specify that the triazoles and imidazole derivatives indicated above are fungus-static drugs; this means that they are limited to blocking the replication and proliferation of the pathogen, leaving the immune system to eliminate it from the organism. patient (these are drugs that do not directly cause the death of the fungus).
This aspect is very important, because it involves a slow recovery process, which ends positively only by strictly adhering to drug therapy (a "possible interruption of administration, in fact, is associated with relapses).
How to cure vaginal candida?
The treatment of vaginal candida is based first of all on the use of antifungal drugs; secondly, it provides for the temporary abstention from sexual activity and particular attention to personal hygiene, nutrition and lifestyle.
Vaginal Candida Medications
Generally, in the presence of vaginal candida, the doctor limits himself to prescribing a local drug therapy, ie based on vaginal pessaries and creams; more rarely, he associates local drug therapy with a systemic one based on taking tablets by mouth.
Among the locally administered antifungal drugs, clotrimazole, econazole, fenticonazole nitrate, miconazole and nystatin are reported; among the oral antifungal drugs, on the other hand, are fluconazole and itraconazole.
For drug therapy to have an effect on vaginal candidiasis, it is essential that it is early and that the patient adheres strictly to it.
Vaginal Candida and Abstention from Sexual Activity
Although the use of condoms prevents the transmission of vaginal candida, doctors advise to avoid sexual intercourse with the partner for the duration of the treatment and to resume only after recovery.
It should be noted that the condom and the contraceptive diaphragm are sensitive to topical antifungals and to vaginal antimitotics, where by sensitive we mean that they could be damaged; any damage to these methods of contraception could be not only a cause of transmission of vaginal candida (in the case of condoms), but also of an unsolicited pregnancy.
Nutrition and Vaginal Candida: what to eat, what not to eat and supplements
Nutrition often plays a crucial role in preventing the re-onset of vaginal candidiasis (recurrence).
Indeed, since Candida it feeds on sugars, for a certain period it would be better to abolish or at least drastically reduce foods containing refined sugars, such as sweets, sweets, industrial fruit juices and other sugary drinks.
Furthermore, it is also often recommended to avoid leavened foods, such as bread, focaccia, pizza and desserts of all kinds.
As for the recommended foods, green light for fruit and vegetables, whole grains, yogurt and lactic ferments; the latter, in particular, are important for the restoration and balance of the microbial flora, thus being useful both in the therapeutic and preventive fields.
Among the fruit, the non-sugary one should be preferred, thus limiting grapes, bananas, figs and candied dried fruit.
Clearly, the diet should be tailored to the individual patient by the doctor or a nutritionist based on the individual condition.
Among the potentially useful supplements we also remember glutamine, an important nutrient both for the cells of the intestine and for those of the immune system, and immunostimulating and adaptogenic phytotherapeutic drugs, such as Echinacea, Uncaria tomentosa and Eleutherococcus.
Did you know that ...
Precisely for those suffering from vaginal candidiasis, there are preparations of lactobacilli (lactic ferments) to be applied directly in the vaginal area.
Vaginal Candida, Lifestyle and Alternative Medicine
As often happens in the presence of rather common diseases with a tendency to become chronic, candidiasis represents a fertile ground for naturopathy and other alternative or complementary medicines.
Remembering that the position of mainstream medicine is definitely critical of these alternative approaches, a little common sense is often enough.
Without disturbing phantom points of vital energy or intoxicating scents, it is clear, for example, how conditions of excessive and prolonged stress can weaken the immune system. The constant practice of physical exercise, regular night rest, careful nutrition avoiding excesses, optimal stress management, and why not also the anti-stress massage performed by expert hands, can certainly benefit the patient suffering from chronic vaginal candidiasis. .
Vaginal Candida and Personal Hygiene Care
As far as personal hygiene is concerned, this must be scrupulous, but at the same time delicate, so as not to alter the balance of the skin and mucous membranes.
The intimate cleanser must in any case be specific and not too aggressive, therefore free of fragrances or other potential allergenic agents.
If in doubt, it is always useful to ask your gynecologist or pharmacist for advice.
Finally, it is good to wear cotton underwear and avoid nylon, microfiber garments and clothes that are too tight; this because Candida it grows more in an anaerobic environment (ie devoid of air) and nylon or microfiber garments and those that are too tight prevent normal skin transpiration.