Chlamydia is an infectious disease caused by the bacterium Chlamydia trachomatis.

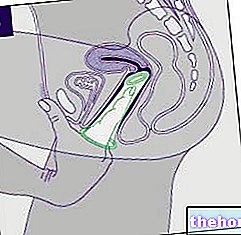
Chlamydia can also be transmitted from the mother to the fetus.
It is often asymptomatic or barely perceptible. The first symptoms appear one or two weeks after the infection.
It is usually not serious, but in some cases it causes genital lesions of considerable importance (inflammation, progress of infection and ascent; sometimes even permanent sterility).
Together with trichomoniasis and gonorrhea, it is among the most common venereal diseases in the world. It mainly affects sexually active individuals who are around 20 years of age.
The published material is intended to allow quick access to general advice, suggestions and remedies that doctors and textbooks usually dispense for the treatment of Chlamydia; such indications must in no way substitute the opinion of the attending physician or other health specialists in the sector who are treating the patient.
What to do
- Prevent chlamydial infection (see prevention below).
If you experience one or more of the following symptoms, you should see your doctor right away.
- Regarding the reproductive system, chlamydia can manifest itself with:
- Abnormal mucus-serous or blood discharge (even away from the period), from the vagina or penis
- Intimate itching
- Pain when urinating
- Testicular discomfort.
- Sometimes small reddish patches appear on the mucous membranes, which can develop into ulcers, lymphogranulomas and fistulation.
- Regarding the anus and rectum, chlamydia can manifest itself with:
- Anorectal pain.
- Anal spasms.
- Urgent need to defecate.
- Bleeding.
The diagnostic process is not very complex and is limited to:
- Collection of a cervical, urethral, vaginal or urinary sample / swab to be analyzed in the laboratory to confirm the identification of the pathogen in question.
What NOT to do
- Engaging in unprotected sex with casual partners.
- Having unprotected oral sex with casual partners.
- Practicing cunnilingus and anilingus (as they cannot be of the protected type) with occasional partners.
- Ignore any symptoms that could signal a "chlamydial infection."
- Consuming sexual intercourse (including cunnilingus and anilingus) in the presence of symptoms that could characterize chlamydial infection.
- Delay the medical check-up.
- Do not carry out a specific investigation with swab analysis; the risk is to confuse the infection with other similar ones (gonorrhea, trichomoniasis, etc.).
- Not following drug therapy correctly and not carrying out checks at the end of the course; the risk is that of incomplete healing and relapse.
What to eat
There is no diet that can cure or prevent chlamydia.
On the other hand, certain nutrients are necessary to support the immune system; some also exert an antioxidant effect and help prevent free radical stress by improving the general condition.
- Vitamin C or ascorbic acid: it is mainly contained in sour fruit and raw vegetables. In particular: peppers, lemon, orange, grapefruit, tangerine, parsley, kiwi, lettuce, apple, chicory, cabbage, broccoli etc.
- Vitamin D or calciferol: it is mainly contained in: fish, fish oil and egg yolk.
- Zinc: it is mainly contained in: liver, meat, milk and derivatives, some bivalve molluscs (especially oysters).
- Selenium: it is mainly contained in: meat, fish products, egg yolk, milk and derivatives, enriched foods (potatoes, etc.).
- Magnesium: it is mainly contained in: oil seeds, cocoa, bran, vegetables and fruits.
- Iron: it is mainly contained in: meat, fish products and egg yolk.
- Polyphenolic antioxidants (simple phenols, flavonoids and tannins): they are mainly contained in: fresh fruit and vegetables, but also red wine, seeds, aromatic herbs, tea, roots, cocoa, officinal herbs, etc.
- Lysine and glycine amino acids: they are mainly contained in: meat, fish products, cheeses and legumes (especially soy).
- Probiotics: they are mainly contained in fermented foods such as yogurt, tofu, tempeh, buttermilk etc.
- Omega 3: they are mainly contained in: oily fish, some oil seeds and related oils, algae.
What NOT to Eat
There are no less recommended products than others for the prevention and treatment of chlamydia. However, it is recommended to avoid:
- Single-issue diets.
- Vegan diet.
- Carnivorous diet.
- Diet free of vegetables and greens.
- Diet based exclusively on cooked and / or preserved foods.
NB. These recommendations are aimed at ensuring the supply of nutrients useful for maintaining the immune system.
Natural Cures and Remedies
There are no natural remedies useful for chlamydia.
The only safe and effective treatment is pharmacological.
However, antibiotics damage the intestinal flora; in this case, it can be very useful to take specific food supplements to keep it alive and active.
- Probiotic supplements: bifidobacteria, lactobacteria and eubacteria are based. They are used orally on an empty stomach and for at least two weeks.
- Prebiotic supplements: they mainly consist of oligosaccharides, unavailable carbohydrates and fibers. It is necessary that they nourish the intestinal bacterial flora and favor the development of that symbiota.
It may be useful to take advantage of herbal remedies based on immunostimulating plants; the most common forms of intake are extract, decoction and essential oils. Not being responsible for harmful drug interactions, they can also be taken at the same time as antibiotics:
- Androgafis.
- Astragalus.
- Echinacea.
- Eleutherococcus.
- Mistletoe.
- Uncaria.
- Cordyceps.
- Garlic.
- Aloe gel.
- Turmeric.
Pharmacological treatment
Antibiotic therapy; your doctor may decide to use one or more of the following drugs:
- Macrolides:
- Azithromycin: for example Azithromycin, Zitrobiotic, Rezan and Azitrocin. A single dose may be sufficient.
- Erythromycin: for example Erythrocin, Erythro L and Lauromycin.
- Penicillins:
- Amoxicillin: for example Amoxicillin, Amoxil and Trimox, Zimox and Augmentin.
- Tetracyclines:
- Doxycycline: for example Doxycicl, Periostat, Miraclin and Bassado. The treatment lasts at least 7-10 days.
- Tetracycline eg Tetrac C, Pensulvit and Ambramycin.
- Quinolones:
- Ofloxacin eg Exocin and Oflocin.
- Levofloxacin eg Levofloxacin, Tavanic, Aranda and Fovex.
- Sulfonamides:
- Sulphysoxazole.
NB. It is important that the treatment be extended to all sexual partners in order to avoid the spread of the disorder. For more information read: Drugs against Chlamydia
Prevention
- Annual screeneng, especially for women.
- With new or non-casual sexual partners, engage only in intercourse protected by a condom.
- With new or non-casual partners, avoid unprotected oral sex
- With new or non-casual partners, always avoid cunnilingus as well as anilingus (as they cannot be of the protected type).
Medical Treatments
Apart from pharmacological ones, there are no other medical treatments for chlamydia.