Generality
The treatment of ascites depends above all on the causes that produced it; for example, in the presence of carcinomas, surgical resection of the neoplasm is necessary, or therapies such as radio or chemotherapy.
Since ascites has cirrhotic origins in most cases, we now focus on the treatment of ascites patients who are affected by this disease.
Diet and general indications
- Bed rest: upright posture activates the renin-angiotensin system, worsens renal perfusion and sodium excretion (aggravation of ascites). On the other hand, bed rest tends to improve the response to diuretics and increases the blood supply to the liver, facilitating its work and restoring normal function. Frequent changes in position and the use of soothing lotions prevent the appearance of ulcers from decubitus.
-
Low-sodium diet: limit the addition of salt to foods and moderate the consumption of those richer in this mineral (such as seasoned meat and fish, and various snacks). Sodium restriction, however, must not affect the palatability of foods (possibly can replace salt with spices), therefore the nutrition, often already deficient, of the cirrhotic patient. The use of low-sodium salt must be agreed with the doctor, as it may require an adjustment of the pharmaceutical doses.
- Water restriction: in the advanced stages of liver cirrhosis there is, in addition to the intense sodium-retention, a deficit of secretion of free water. Consequently, due to the hypervolemia there is a reduction in the concentration of sodium in the blood. The therapy of this dilution hyponatremia classically consists of water restriction.
- Stop the consumption of alcohol and minimize the use of NSAIDs (unless otherwise prescribed). Consume small and frequent meals, an adequate protein intake is also important, but must be reduced in the presence of hepatic encephalopathy.
Medicines
For further information: Medicines to cure Ascites
Diuretics are intended to reduce blood volume and with it portal pressure. Usually: spironolactone (aldactone) and furosemide (lasix) are used. The first is a potassium saver (aldosterone antagonist, which increases sodium elimination and conserves potassium), the second is not.
The starting dose is 40 milligrams per day for furosemide and 100 mg for spironolactone; these dosages can be increased up to the respective maximum level of 160 and 400 milligrams. The combined intake of these medications in the morning is typically recommended to prevent annoying frequent urination at night.
The undesirable effects of spironolactone are due to its antiandrogenic action and include decreased libido, impotence and gynecomastia (possibly controlled through the concomitant use of tamoxifen or by replacing it with its hydrophilic derivative potassium canrenoate). Furthermore, the increase in blood potassium may limit the use of this drug in the treatment of ascites. High doses of furosemide may instead cause electrolyte disturbances and metabolic alkalosis.
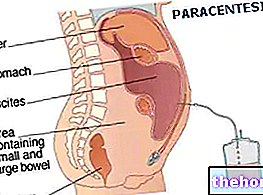
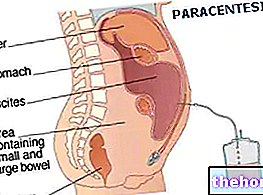
Therapeutic paracentesis
All patients who do not tolerate the aforementioned diuretic regimens at dosages such as to produce the desired effects are candidates for this intervention. Therapeutic paracentesis has the purpose of emptying the abdominal cavity of ascitic fluids, with the aid of a small needle inserted in the abdomen of the patient in sterile conditions; this allows to quickly remove large quantities of fluids. During paracentesis, the simultaneous re-expansion of the plasma volume is often necessary, by infusing special solutions containing albumin; this maintains the balance of the vaso-circulatory system by antagonizing the vasoconstriction exerted by the subtraction of fluids.
Therapeutic (or evacuative) paracentesis is the first choice approach for the treatment of refractory ascites.
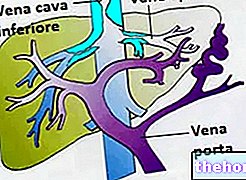
Intrahepatic transjugular portosystemic shunt (TIPS)
A long needle is inserted, under local anesthesia, through the jugular vein in the neck, and pulled down to the hepatic vein, then into a branch of the portal vein in the liver. The operation consists in placing a metal prosthesis between the hepatic vein and the right or left branch of the portal vein (porto-systemic shunt); the stent will serve to maintain the patency of the shunt created over time. Not all patients are suitable for this type of intervention, which aims - often with a decisive outcome - to significantly reduce portal hypertension.
Liver transplantation
The development of ascites is associated with 50% mortality in the two years following diagnosis. Once ascites becomes refractory to medical therapy, 50% of patients die within six months. Therefore - despite improvements in medical therapy in therapeutic paracentesis and shunt surgery - survival is often not improved without transplantation. Therefore, for patients with ascites the hypothesis of transplantation must be taken into consideration, which however represents a very complicated and prolonged intervention, which requires careful and constant monitoring by a specialized medical staff.
Other articles on "Ascites: Care and Treatment"
- Ascites: Symptoms and Diagnosis
- Acite
- Ascites - Medicines for the treatment of Ascites