Definition
From the Greek "tachys-kardia"(Lit." accelerated heart "), we speak of tachycardia when the heart rate (HR) in conditions of rest exceeds the normal range (for the reference population). For the adult, tachycardia occurs when the resting HR exceeds 100 beats per minute (bpm); the opposite phenomenon is bradycardia.
Causes
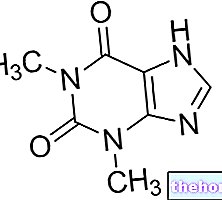
Tachycardia reflects cardiac alterations related to the production of electrical signals: in other words, when the physiological electrical-cardiac activity is altered for any reason, the probability that tachycardia occurs increases. The following are the most common predisposing factors: abuse of coffee, nerve substances and drugs, alcoholism, anemia, anxiety, electrolyte disturbances, intake of anti-asthma and antihistamines, excessive emotions, fever, heart attack (including previous ones), hypertension, hyperthyroidism, malformations congenital affecting the heart.
Symptoms
In the presence of tachycardia, the heart is unable to effectively pump blood to all parts of the body; therefore, some organs may require oxygen. Similar conditions can cause: heartbeat, chest pain, shortness of breath, palpitations, fainting , dizziness.
- Complications: sudden cardiac arrest, increased risk of stroke, myocardial infarction, death
The information on Tachycardia - Tachycardia Treatment Drugs is not intended to replace the direct relationship between healthcare professional and patient. Always consult your doctor and / or specialist before taking Tachycardia - Tachycardia Treatment Medications.
Medicines
It is not certain that all tachycardia sufferers complain of the characteristic symptoms of the disease: in fact, a mild or occasional tachycardia (for example dependent on anxiety or an "excessive emotion) should not alarm excessively, although a doctor's consultation is always recommended.
We must not forget, in fact, that tachycardia can also cause serious consequences, even leading to death.
The main objective of the treatment of tachycardia is therefore the slowing of the heart rate, which can be achieved through several treatment options:
- Administration of specific drugs (listed in detail in the next paragraph)
- Implementation of medical maneuvers (e.g. Valsalva maneuver)
- Application of ice packs to the face
- Electroconversion with the defibrillator (in extreme cases)
- Surgical ablation: insertion of micro leads inserted into the blood vessels, which reach the heart
- Implantation of cardioverter-defibrillators or peacemakers: small electrical devices capable of restoring the physiological heart rate by blocking tachy-artyms in the bud
The following are the classes of drugs most used in tachycardia therapy, and some examples of pharmacological specialties; it is up to the doctor to choose the most suitable active ingredient and dosage for the patient, based on the severity of the disease, the state of health of the patient and his response to treatment:
Antiarrhythmic drugs: when medical maneuvers are not sufficient to restore heart rate values, it is possible to intervene with antiarrhythmic drugs:
- Propafenone (eg. Rytmonorm, Propafenone DOC, Cardiofenone): start treatment for the treatment of tachycardia with a drug dose of 150 mg, to be taken orally every 8 hours. It is also possible to take the drug formulated as slow-release tablets: in this case, take 225 mg every 12 hours. For the maintenance dose, it is possible to increase the dosage every 3-4 days to 225-300 mg every 8 hours for immediate-release tablets, or increase the dosage to 325-425 mg to be taken every 12 hours for the slow-release tablets. release (at least 5 days after the start of treatment). Consult your doctor.
- Amiodarone (eg Angoron, Cordarone, Amiodarone ZTV): the drug is also indicated for the treatment of supraventricular tachycardia in children. Indicatively, for infants less than one month old suffering from tachycardia, it is recommended to take 10-20 mg / kg of active ingredient per day orally, possibly dividing the load into two doses. Repeat for 7-10 days. After this period, it is possible to reduce the dosage by 5-10 mg, and repeat the treatment for 2-7 days, according to the patient's response. It is also possible to administer the drug intravenously (5mg / kg in 60 minutes). For children over one year of age suffering from tachycardia, it is recommended to administer 10-15 mg / kg of the drug orally, for 4-14 days, in two doses per day. The maintenance dose suggests taking 5-10 mg / kg orally, once a day.
- Adenosine (eg Adenoscan, Krenosin): start therapy with a drug dose of 6 mg, intravenously; then follow with 20 ml of physiological solution. If, after a couple of minutes, the patient does not benefit from the therapy, it is recommended to proceed with a "further dose of drug (12 mg), to be repeated twice if necessary.
- Mexiletine (eg Mexitil): start therapy with a drug dose of 200 mg, to be taken orally every 8 hours, when the body is unable to maintain normal heart rate values. Prolong therapy for at least 2-3 days, even if symptoms disappear.
- Lidocaine (eg. Xylocaine, Lidoc C BIN, Xilo MYNOL, Basicaina, Lidoc C / NOR B SAL): start therapy with a drug dose (analgesic-antiarrhythmic) at a dose of 1-1.5 mg / kg by intravenous injection . Further doses of 0.5-0.75 mg / kg can be repeated every 5-10 minutes. Do not exceed 3 mg / kg. Thereafter, continue therapy with continuous intravenous infusion (1-4 mg / min). If IV infusion is not possible, a loading dose of the drug can be administered intravenously, increasing the dose by 2-2.5 times compared to what should be taken intravenously.
Calcium antagonists and beta blockers: these are two main classes of drugs used in therapy for the treatment of arterial hypertension; they can also be used in therapy for the prevention of tachycardia episodes, especially in predisposed patients.
Calcium antagonists:
- Diltiazem (eg Altiazem, Tildiem, Diladel): for the treatment of tachycardia, start with a drug dose ranging from 30 to 60 mg, to be taken 3-4 times a day. The maintenance dose involves taking 180-360 mg of the drug orally per day, in equally divided doses over 24 hours.
- Verapamil (eg Isoptin, Kata): indicatively, for the treatment of tachycardia, take 5-10 mg of the drug as an IV bolus. at least 2 minutes. 30 minutes after the first dose, repeat the administration taking 10 mg (when the initial response is inadequate). Subsequent doses should be determined by the physician based on the patient's response to treatment.
Beta blockers:
- Metoprolol Tartrate (eg. Seloken, Lopresor, Metoprolol AGE): for the treatment of tachycardia, start treatment with a dose of active ingredient equal to 100 mg, to be taken orally, in 1 or 2 doses. The maintenance dose suggests an administration of active equal to 100-450 mg per day. Slow-release formulations must be taken once per 24 hours.
- Esmolol (eg. Brevibloc): start therapy against tachycardia with a drug dose of 500 mcg / kg over one minute. The maintenance dose involves administering the drug at a dose of 50 mcg / kg / min for 4 minutes Consult your doctor for more information.
- Nadolol (eg Corgard): It is recommended that tachycardia therapy be initiated with a drug dose of 40 mg, to be taken by mouth once a day. Continue with a maintenance dose of 40-80 mg, always to be taken in the same way as described above. Some patients may need high dosages, up to a maximum of 320 mg per day: the precise dosage clearly depends on the patient's general health condition and the severity of the tachycardia.





















-nelle-carni-di-maiale.jpg)




