Characterized by the use of catheters supplied with balloons, angioplasty is one of the therapeutic applications performed in interventional hemodynamic laboratories, present in major hospitals.
Synonyms for Angioplasty
Angioplasty is also known as percutaneous angioplasty.
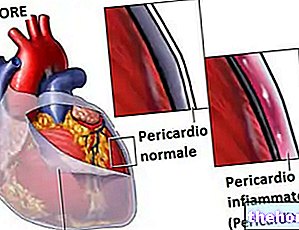
or thrombosis phenomena, or as a result of inflammatory processes.Angioplasty aims to restore, as far as possible, the blood flow inside vessels whose patency is compromised by the presence of an atherosclerotic plaque, a thrombus or a vascular inflammation.
Narrowing and occlusions of blood vessels are an example of vascular stenosis.
What is Atherosclerosis?
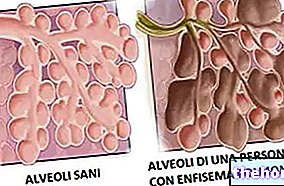
Atherosclerosis is the phenomenon of hardening of medium and large caliber arteries, which over time induces the formation of atheromas on the inner wall of the arterial vessels just mentioned.
Also known as atherosclerotic plaques, atheromas are aggregates of lipid (especially cholesterol), protein and fibrous material which, due to the position occupied, are an obstacle to normal blood flow inside the arteries; moreover, they can be the subject of inflammatory processes, which cause its fragmentation and dispersion in other blood vessels - this time smaller - with consequent occlusive phenomena.
Angioplasty: When To Do It?

Angioplasty is a feasible treatment in the presence of:
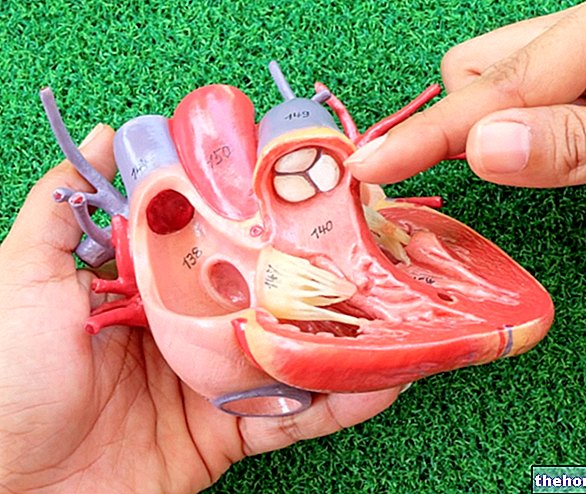
- Narrowing or occlusions of the coronary arteries of the heart. The presence of these problems is known by the more general term of coronary heart disease.
- Narrowing of the great arteries due to atherosclerosis.
- Peripheral arterial disease. It is the vascular disease characterized by the narrowing of the arterial vessels of the limbs (upper or lower) and the organs of the trunk.
- Carotid stenosis. It is the narrowing or occlusion of one or both carotids, ie the arterial vessels that develop from the aorta towards the neck to carry oxygenated blood to the brain.
- Narrowing or occlusions of the veins of the thorax, abdomen, pelvis or limbs (upper or lower).
- Narrowing of the renal arteries associated with renovascular hypertension. The latter affects renal function.
- Stenosis of the arteriovenous fistula in patients requiring hemodialysis.
Coronary Angioplasty: What is it and Who is it for?
When it is aimed at the elimination of stenosis present inside the coronary arteries, angioplasty is more properly called coronary angioplasty, or percutaneous transluminal coronary angioplasty.
Coronary angioplasty is a procedure that may be indicated for:
- People with patency problems in the coronary arteries, who continue to have symptoms such as angina pectoris and dyspnoea, even in spite of drug therapies and an improvement in lifestyle;
- Individuals with an ongoing heart attack (or myocardial infarction);
- People at risk of heart attack.
The use of the conditional is mandatory, as coronary angioplasty is applicable only to a particular fringe of patients falling within the categories listed above: in fact, those with mild-moderate and limited coronary artery disease are suitable for the procedure. to one or a few coronary arteries.
For further information: Coronary Angioplasty: What is it for and How is it performed?Peripheral Angioplasty: What is it and what is it used for?
"Peripheral angioplasty" and "percutaneous peripheral angioplasty" are the terms that define angioplasty procedures aimed at treating stenosis due to "peripheral arterial disease."
Carotid Angioplasty: What is it and what is it used for?
As the name suggests, carotid angioplasty is the angioplasty procedure reserved for patients with carotid stenosis.
Venous Angioplasty: What is it and what is it used for?
Venous angioplasty is the intervention of angioplasty that can be carried out in the presence of stenosis of the arteriovenous fistula or narrowing of the venous vessels.
and, sometimes, an electrocardiogram) and a thorough study of the clinical history; the latter in particular aims to clarify the patient's general state of health, if the latter is following any drug therapy, if he has allergies to drugs, sedatives, etc. and if you are pregnant (in the case, of course, it is a woman of childbearing age).
The clinical tests that precede an angioplasty are used to establish if there are contraindications to the procedure or particular risks and if the patient is suitable to undergo the operation.
Angioplasty: what to do before surgery
On the day of an angioplasty, it is generally expected that the patient has fasted for at least 6-8 hours, which means that, if the procedure is set for the morning, the last meal allowed is that of the previous evening.
Furthermore:
- If the patient is undergoing some anticoagulant drug therapy, it is likely that in view of the angioplasty the interventional doctor will ask him to temporarily suspend the treatment and to resume it only on his instructions.
- If the patient follows pharmacological therapies different from the previous ones on a daily basis, he is invited to bring the various medicines with him to the hospital, for the day or days of hospitalization that could follow the intervention.
- The patient must organize his return home, asking for help from a family member or a friend, as after the operation he could feel debilitated.
Angioplasty: how is the procedure carried out?
There are essentially six salient moments of a generic angioplasty; here they are briefly in chronological order:
- Positioning and sedation of the patient, and monitoring of his vital functions;
- Creation of a vascular access point and insertion of a guide wire for the diagnostic catheter;
- Insertion and positioning of the diagnostic catheter, and injection of the contrast medium;
- Conduction at the site of obstruction / narrowing of the balloon catheter;
- Inflating the balloon and sometimes applying a stent;
- Extraction of catheters and guide wire, and conclusion of the procedure.
Patient positioning
First, the patient must undress and put on a gown specially prepared for him; together with the clothes, he must also remove any glasses, watch, various jewels, etc.
Then, once he has put on the gown, he is instructed by the medical staff to sit on the X-ray table on which, subsequently, the interventional doctor will perform the angioplasty.
Sedation
Sedatives are administered through a needle-cannula usually inserted on a patient's forearm.
The pain caused by the insertion of the needle-cannula is minimal, sometimes imperceptible.
Sedation serves only to promote relaxation of the patient; the latter, therefore, remains conscious, even if sleepy, for the entire duration of the procedure.
Sometimes, the administration of sedatives is accompanied by that of anticoagulants; the purpose of the latter is to prevent the formation of blood clots due to the subsequent passage of the various catheters.
Monitoring of vital functions
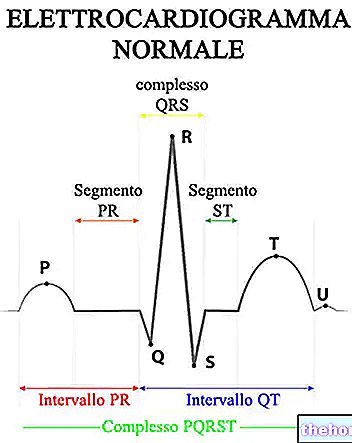
After the sedation, an assistant to the specialist physician is responsible for connecting the patient to medical instruments that are used to measure and monitor blood pressure, heart rate and blood oxygen saturation.
The monitoring of the aforementioned vital parameters serves to detect in time any problems that may occur during angioplasty.
Creation of the Access Point
The access point is a small perforation made in an artery and guaranteed by a sort of needle-cannula, which serves to introduce, at the vascular level, the guide wire, the diagnostic catheter and the balloon catheter.
In an angioplasty, the point of access may be located on the femoral artery at the level of the groin or on the brachial artery.
It should be noted that, before practicing the access point, the interventional doctor, with his collaborators, will wash and disinfect the area of interest and, subsequently, inject a local anesthetic (to reduce the discomfort induced by the procedure drilling).
Inserting the Guide Wire
Once the access point has been created, the interventional doctor introduces a very thin and flexible metal wire, simply called the guide wire; after which, he starts the X-ray instrumentation and, with the support of the images provided by the latter, he proceeds to lead the guide wire near the obstruction / narrowing.
The purpose of the guide wire is to act as a sort of railway track on which to transport the diagnostic catheter near the vascular obstacle.

Insertion and Conduction of the Diagnostic Catheter in the Narrowing site
Once the guide wire has been positioned, it is the turn of the diagnostic catheter: the interventional doctor inserts it into the vascular system through the access point on the femoral or brachial artery and leads it to the vicinity of the narrowing with the help of the guide wire.
Normally, the operation of conducting the diagnostic catheter to the heart is not painful and does not cause other particular sensations; however, if this is not the case and the patient feels some kind of discomfort, it is important to communicate it immediately.
Injection of the contrast medium
After placing the diagnostic catheter, the interventional physician injects through it a contrast agent visible on X-rays, which, once diffused in the vessels where it has been placed, shows the vascular obstruction / narrowing on a monitor.
In this case, the patient distinctly perceives the release of the contrast medium: at the "injection of the latter", in fact, he feels a sort of flush of heat, which with the English term is called flashing.
Balloon Catheter Insertion
Having identified the impediment to the blood flow, the interventionist introduces a very thin probe inside the diagnostic catheter and leads to the obstruction / narrowing site, equipped at the end that penetrates the vascular system with an expandable component, called a balloon; this probe is the most often mentioned balloon catheter.
Fundamental for the proper conduction of the balloon catheter are the X-ray instrumentation and the diagnostic catheter - guide wire (the latter allow to direct the balloon catheter where the obstruction resides).
Inflating the Balloon
Once the balloon catheter has been positioned, the interventional doctor inflates and deflates the balloon; the latter, at the moment of expansion, pushes the vascular obstacle against the walls, restoring the patency of the blocked / restricted blood vessel.
Sometimes, to get a better result, you may inflate and deflate the balloon several times.
Inflation of the balloon could cause a feeling of discomfort to the patient; this sensation, however, is temporary and disappears as soon as the balloon deflates.
Application of one Stent
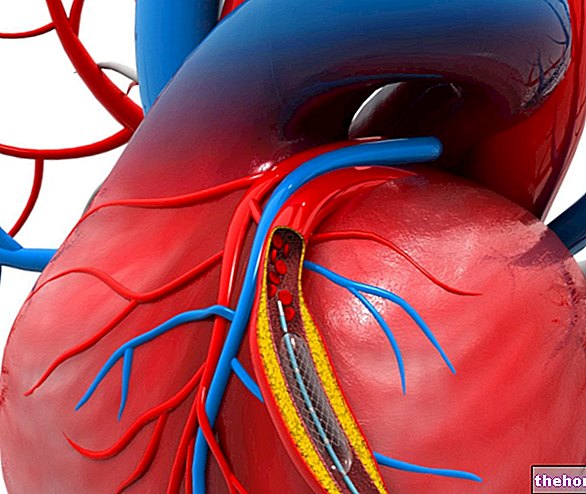
Now more and more often, the inflation of the balloon is followed by the application of one stent; the stent they are small expandable cylinders with metal meshes, which serve to keep blood vessels open with a tendency to occlude / narrow.
Basically, the application of one stent has the purpose of prolonging the effects deriving from the inflation of the balloon.
Extraction of the Catheters and Conclusion
Once the interventional physician has restored vascular patency, angioplasty can be considered almost over.
To ratify the conclusion are the extraction of the various catheters and the guide wire, followed by the tamponade of the access point.
Angioplasty: How Long Does It Last?
Angioplasty procedures can last from one to more than two hours, depending on the extent of the narrowing / obstruction.
, however, it is recommended to periodically check the appearance of the wound.Angioplasty: recovery times
If the operation is successful, recovery times from a scheduled angioplasty are approximately one week.
This timing is lengthened, sometimes even considerably, in the event of complications or when the procedure is in an emergency regime (eg: heart attack in the case of a "coronary angioplasty).
What to do after an angioplasty
After an "angioplasty, it is indicated:
- Drink plenty of water to speed up the elimination of the contrast medium from the body;
- Rest for at least a week;
- Undergo periodic checks;
- Follow your doctor's instructions regarding:
- The drugs granted and indicated. Among the drugs indicated, anticoagulants could be included: these are used to prevent thrombo-embolic phenomena, a possible risk of angioplasty procedures;
- When to go back to work;
- How to keep the wound that results from the access point clean;
- When to resume various daily activities.
- Permanently adopt a healthy lifestyle.
What not to do after an angioplasty
After an "angioplasty, it is a good idea to:
- Avoid any strenuous activity for several days;
- Avoid driving in the first 24 hours following the intervention;
- Avoid full showers and baths for at least the first week (precaution to prevent the wound from reopening).
When to contact the doctor after an angioplasty?
After an "angioplasty, the patient should contact the interventional physician immediately or go to the nearest hospital if:
- The entry point bleeds (hemorrhage) without a hint of stopping and / or swells. In case of bleeding, a temporary remedy pending treatment is to press on the wound.
- The pain at the wound increases rather than decreases.
- The wound becomes infected. The classic signs of infection are skin redness and fever.
- Symptoms such as weakness, fainting, chest pain (after a "coronary angioplasty), etc. are persistently present.
Serious Complications
- Thrombo-embolic phenomena induced by the passage of the diagnostic catheter along the vascular system. In some types of angioplasty (eg coronary angioplasty), these thrombo-embolic phenomena can be responsible for myocardial infarction or ischemic stroke).
- Vascular damage to the arteries crossed by the diagnostic catheter.
- Return of the obstruction / occlusion.
- Formation of blood clots due to stent.
- Kidney damage. It is due to the contrast medium.
It should be noted that, depending on the type of angioplasty, other more specific complications can be added to the complications listed above (eg: cardiac arrhythmia, in the case of coronary angioplasty).
Angioplasty: Who is most at risk of complications
During an "angioplasty, the risk of complications increases by factors such as:
- The advanced age;
- Carrying out the procedure without "adequate preparation (happens in emergencies);
- The presence of severe kidney disease;
- The presence of severe heart disease.
It should be noted that, depending on the type of angioplasty, other more specific ones can be added to the contraindications listed above.