Causes
Although a precise cause of origin is not known, it is conceivable that endometrial polyps are the final result of an abnormal response to estrogenic hormonal stimuli. Premenopausal women are the category most at risk for endometrial polyposis.

Symptoms
Endometrial polyps can develop completely asymptomatically. Sometimes, however, the presence of a polyp in the endometrium can cause dyspareunia and menstrual discomfort (irregularity, hypermenorrhea, menorrhagia, dysmenorrhea, spotting).
Diagnosis
Endometrial polyps can be confirmed by different investigative investigations, such as sonosalpingography, hysterosalpingography, curettage and hysteroscopy.
Therapy
Drug therapy (with progestins or gonadotropins) is not always effective. Most often, endometrial polyps are removed by hysteroscopy. In case of malignant evolution, we proceed with hysterectomy (removal of the uterus).
: for this reason, in the common jargon, the terms "endometrial polyps" and "uterine polyps" are used interchangeably.
Endometrial polyps are a particularly frequent phenomenon in women during the period immediately preceding menopause. In fact, it is estimated that the incidence of endometrial polyps increases as we age, and then decreases considerably after menopause.

- Polyps in the endometrium rarely appear around the age of 20-30, just as the disorder is unlikely to occur after menopause.
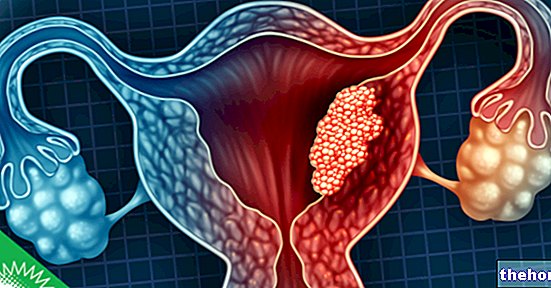
These polyps can adhere to the uterine wall by means of a pedicle, which allows the polyp to protrude into the vagina when it reaches a considerable size.
The sessile endometrial polyps (also called "broad-based") have no peduncle and adhere to the uterine mucosa with a small root; therefore they cannot protrude into the vagina.
of estrogen.
For this reason, women aged between 40 and 50 years (PRE-menopausal period), presenting a particular estrogenic profile, are more prone to the formation of polyps in the endometrium.
To understand...
Plasma hormone levels in premenopausal women cannot be accurately reported as they are subject to large and unpredictable fluctuations. The ovaries undergo a progressive decline right from the premenopause, gradually becoming more atrophic and smaller. As one approaches the actual menopause, the hormonal structure becomes more defined: the levels of estrogen - and especially progesterone - are extremely low, while those of FSH (follicle stimulating hormone) and LH (luteinizing hormone) appear high. After menopause, the formation of endometrial polyps is extremely unlikely due to the hormonal stability that characterizes it.
Clinical evidence shows that endometrial polyps tend to occur more often in obese women, especially when the body mass index is equal to or greater than 30. Furthermore, it seems that women are more exposed to the risk of endometrial polyposis in case of previous (or current) intake of antiestrogens, drugs indicated for the treatment of breast cancer and gynecomastia (e.g. tamoxifen and raloxifene).
In the past it was assumed that hypertension and a previous history of cervical polyps (at the cervix of the uterus) could constitute risk factors for endometrial polyposis. However, a study reported in the journal Journal of Obstetrics and Gynecology this hypothesis was refuted, as no proven and demonstrable association was found.
.
Symptoms tend to occur when polyps take on a considerable size.
The clinical picture of endometrial polyposis is characterized by:
- Pain during sexual intercourse (dyspareunia)
- Menstrual irregularity
- Heavy menstruation (hypermenorrhea)
- Painful menstruation (dysmenorrhea)
- Extremely profuse blood loss during menstruation (menorrhagia)
- Menstruation-like uterine discharge during the postmenopausal period
- Bloody vaginal discharge after intercourse
- Spotting (loss of dark uterine blood that interposes between two periods)
The symptoms described above must be carefully evaluated by the gynecologist, since they are almost the same as those that occur during endometrial cancer. Consequently, an accurate differential diagnosis is essential.
Most uterine polyps constitute a benign condition: the probability of degeneration into tumor forms is very low (<1%).
: the uterine polyp, by obstructing the tube openings, prevents fertilization of the egg cell.Women with endometrial polyps - especially large ones - in the vicinity of the salpingus can undergo infertility. To overcome this drawback, surgical excision of the cell growth is recommended within the shortest possible time from the assessment.
. The test is performed by transabdominal and transvaginal pelvic ultrasound.
- Progestogens (eg Norethindrone)
- Gonadotropins or releasing hormone agonists (Leuprolide or Goserelin)
The most appropriate therapy for the removal of endometrial polyps is essentially surgical: in fact, the excision of the cell growth favors the complete remission of symptoms. The most used surgical strategies for this purpose are:
- Hysteroscopy - complete surgical removal of the uterine polyp
- Hysterectomy: removal of the uterus, indicated when the uterine polyps contain neoplastic cells
It should be emphasized, however, that the risk of recurrence is real even after a perfectly successful surgery. For this reason, women with a previous history of endometrial polyposis should undergo ultrasound / hysteroscopic checks more frequently.