Definition
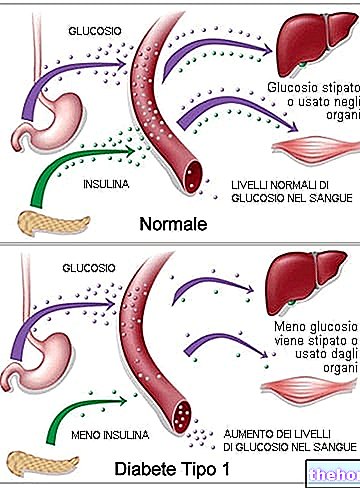
As the term itself anticipates, the diabetic foot (or neuropathic foot) represents a fearful chronic complication of diabetes: it is a morbid state that develops as a consequence of neuropathy * and arteriopathy *, typical pathological conditions of the original metabolic disease.
* Glossary- Neuropathy: alteration of the peripheral nervous system which mainly manifests itself with tingling, cramps, gait disorders and altered sensitivity (inability to perceive pain, heat and cold)
- Arteriopathy: a pathological condition that refers to problems with blood circulation in the arteries (poor blood circulation)
Neurological damage (i.e. the diabetic neuropathy) can cause numbness or loss of the ability to sense pain and temperature changes in the lower extremities. What has been said means that a diabetic patient tends not to notice the presence of cuts, wounds, burns, frostbite and so on at the level of the feet precisely because his defense response to pain is weakened.
If, in addition to diabetic neuropathy, poor circulation in the lower limbs is added (arteriopathy and vascular lesions), it is easy to understand how a small scratch on the foot can cause exaggerated damage, bleeding ulcers which, in the long run, can induce gangrene.

An uncontrolled and dangerously underestimated diabetes constitutes a real risk not only for the health of the feet but also for the patient's life itself.
Neuropathy and diabetic foot
Neuropathy is extremely dangerous for a diabetic patient's feet. In the presence of a foot injury, the patient - who feels less discomfort than the actual extent of the damage or does not perceive it at all - continues to put weight on the foot and walk inadequately: this behavior worsens the situation because starting from a small lesion (such as an apparently harmless callus) quickly creates an increasingly large wound which, degenerating, forms bleeding ulcers, infections or gangrene.
Another element not to be overlooked is represented by foot deformities, which may appear even before the onset of the characteristic symptoms of diabetes. This disorder is a consequence of neuropathy: there is therefore a reduction in strength in some groups of muscles (generally the anterior ones of the leg), consequently the other muscles prevail, thus causing a retraction of the foot.
Deepening
What are the warning signs that can suggest a bad blood circulation in a diabetic?
A suspicion of poor or poor blood supply can arise when:
- Abnormal pins and needles are felt in the feet even during rest
- Leg cramps occur even after a short walk
- Small foot wounds cannot heal easily
- Feet take on a different color (become darker, red, blue, green or black)
- You have the sensation of constantly having cold feet
- Calluses often form on the sole of the foot or between the toes
From what has been said it is easy to understand how the feet and toes are forced to modify their support on the ground; therefore the toes, which tend to bend, force the foot to bear abnormal and exaggerated workloads. The fragile skin of the foot, unable to tolerate shocks, rubbing and trauma, tears easily or is affected by calluses and blisters which, if not treated in time, can degenerate into ulcers.
For further information: Diabetic Foot Symptoms
Arteriopathy and diabetic foot
But why doesn't this happen so quickly in a healthy person's feet?
The rapid degeneration into foot ulcers and infections starting from a small lesion in a diabetic patient is explained by poor circulation in the lower extremities (arteriopathy). The feet of a diabetic, not receiving the necessary blood supply, struggle to repair the damage that the skin has suffered.Furthermore, the skin of the diabetic foot becomes thin, fragile and extremely delicate (like the skin of a child), therefore more prone to trauma and injuries of all kinds.
On the other hand, this rapid degeneration of foot injuries does not occur so often in healthy subjects thanks to the ability of the blood to ensure adequate blood circulation even at the level of the feet.
Complications of the diabetic foot
Foot ulcers are undoubtedly the most frequent complication that occurs in the feet of a diabetic. The danger of ulcers is closely linked to the poor circulation induced by peripheral arterial disease of the diabetic: not receiving the required amount of blood, the ulcers struggle to heal. Consequently, a cascade mechanism is triggered that leads to hemorrhages and / or infections. When the infection spreads, the patient runs the risk of tissue death (tissue necrosis), hence gangrene. In the latter case, the limb requires immediate medical-surgical intervention, which involves the administration of antibiotics to kill bacteria, the removal of infected tissue and, when necessary, the amputation of the limb (or part of it) to prevent the damage from spreading to neighboring districts.
Data in hand ...
From the statistics reported in the scientific journal The Journal Of Clinical Investigation it is clear that:
- Foot ulcers occur in 15% of diabetics
- 84% of lower atria amputations in diabetics are precisely related to the development of foot ulcers
The diabetic foot is only the tip of the iceberg, below which there is a series of very dangerous problems that always require medical control and monitoring.
Other articles on "Diabetic Foot"
- Diabetic foot: diagnosis, care and treatment
- Diabetic foot: what to do and what not to do













-nelle-carni-di-maiale.jpg)