Introduction
As thoroughly analyzed in the introductory article, the Papilloma Virus is the protagonist of skin sores of negligible entity, such as warts, and, at the same time, is involved in the manifestation of terrible tumor lesions, such as those in the neck of the uterus. In this discussion, the attention will be focused on the mode of contagion, on the consequences and on the possible medical treatments aimed at the removal of the Papilloma virus.
Papilloma virus infection
To generate infection, the human papilloma virus must enter an epithelial stem cell located on the basement membrane; probably, the entry of the Papilloma virus into the cell is favored by binding to a surface receptor which, however, has not yet been identified with certainty.
On the one hand, the Papilloma Virus has a "high affinity for epithelial cells in differentiation of skin and mucous membranes, on the other hand, HPV has a restricted tropism for the cells that form the multilayered squamous epithelium. Once it has entered the cell nucleus, the Papilloma virus is able to alter the normal cell cycle of the infected cell ; it is observed that in most cases the Papilloma Virus proliferates preferentially inside the granular layer of the skin.
Through the desquamation of the differentiated and superficial layers of the skin and mucous membranes, the virus can be transmitted to other subjects.
The Papilloma virus is normally transmitted by sexual contact; however, it must be emphasized that the virus also proliferates at the level of the shaft of the penis, perineum and groin: for this reason, condoms are often not sufficient to protect the (healthy) partner from contagion, after intercourse with an infected person or carrier.
Remember that in healthy women, with an efficient immune system, HPV infection is often blocked in the bud: the body's defense system, in fact, prevents the virus from causing damage. In some patients, however, the virus remains silent for many years and under favorable conditions it can induce the conversion of "normal" cells (especially the superficial ones of the cervix) into crazed and cancerous cells.
HPV and cervical cancer
The reasons why some women develop cancer following exposure to the Papilloma Virus are not yet so obvious and immediate: clearly, the efficiency of the immune system is a fundamental element to minimize the risk of malignant degeneration. However, some risk factors have been identified that seem to increase the chances of a progression of the superficial lesions of the Papilloma Virus, up to the development of cancer (cervical intraepithelial neoplasia): from an American study, it is shown that women smokers are twice as likely than those who do not smoke to develop cervical cancer. However, it is conceivable that some strains of HPV are more aggressive than others, so they can induce cancer very easily.
It seems that even the prolonged administration of contraceptive pills, the co-presence of other venereal diseases and pregnancy may, in some way, expose the woman to a greater risk of malignant evolution of the lesion.
Papillomavirus (HPV) infections
Problems with playing the video? Reload the video from youtube.
- Go to the Video Page
- Go to Wellness Destination
- Watch the video on youtube
HPV and benign lesions
Warts are the most frequent skin lesions, fortunately benign, caused by the Papilloma virus: these are wart-like growths that preferentially infect hands, feet and genitals following contact with a wart of another person. The showers , humid and crowded environments, as well as high temperatures and humidity are elements that favor the replication and propagation of the Papilloma virus.
Warts caused by the Papilloma virus are classified into:
- Acuminate warts: expression of a sexually transmitted "genital HPV infection. In men, warts occur preferentially in the glans penis, urethral meatus, frenulum, shaft of the penis and balano-preputial sulcus; in women, on the other hand, the areas most involved are the vulva, the neck of the uterus and the vagina. Most of the time, warts are asymptomatic, although some variants generate burning, itching and local irritation.
- Common warts: skin lesions triggered by the Papilloma virus generally have an irregular shape and often (but not always) run asymptomatically.
- Plantar warts: typical of the sole of the foot, these warty lesions caused by the HPV virus are easily transmitted in swimming pools and gyms.
- Flat warts: raised warty lesions: the Papilloma virus, infecting hands, feet, face and legs, can cause these skin damages, which tend to vanish in a short time.
Diagnosis
The diagnostic approach to monitor and control HPV infection, as well as the lesions caused by it, is essentially based on clinical investigation, Pap smear, colposcopy and molecular examination (HPV-DNA).
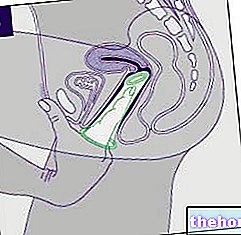
The observation of the lesion by an expert eye is essential to trace a diagnosis, however approximate, of the infection: for female genital warty lesions, a gynecological examination is essential, the diagnosis of which will be confirmed, if necessary, by the "colposcopic examination," essential for obtaining an enlarged and more precise view of the uterine cervix.
In case of doubtful or uncertain diagnosis, it is recommended to proceed with a specific biopsy.
The molecular test, also known as the HPV-DNA test, determines whether or not the viral genome is present, even before the cervical cells develop tumor abnormalities.
Last but certainly not least, the PAP test, now common practice in the majority of gynecological check-ups: it is a cytological examination that allows to identify the alterations of the cells of the uterine section by taking a sample of endocervical cells through a swab .
For sexually active women, it is recommended to undergo PAP testing from the age of 25, every three years, for monitoring and early detection of precancerous damage.
Watch the video
- Watch the video on youtube
Therapy
The therapy for the treatment of HPV infections depends on the type of Papilloma Virus involved in the lesion; for example, when HPV infects the skin and promotes the growth of warts on hands and feet, drug therapy may not even be necessary: in fact, wart sores tend to regress on their own. However, sometimes particularly resistant warts and lasting can be treated with cryotherapy, laser therapy and electrocoagulation. Direct application of drugs such as retinoids, antivirals, immunomodulators and salicylic acid can also accelerate healing times.
The same goes for the treatment of sharp warts: pharmacological and medical treatment (such as surgery, laser therapy, etc.) may not be necessary, especially in the case of asymptomatic and small lesions. As regards the most dangerous papilloma virus infections, implicated in the onset of uterine cancer, the therapy is more problematic: radiotherapy and chemotherapy, possibly associated, favor the death of malignant cells; surgery is recommended for women with early-stage cervical cancer. For further information: read the article on treating cervical cancer.
HPV infection prevention
Vaccine prophylaxis provides a shield from HPV infections: the quadrivalent vaccine exerts good protection against the genotypes involved in the vast majority of benign warty sores, such as genital warts (HPV 6 and HPV 11), and cervical neoplastic lesions (HPV 16 and HPV 18). In some regions of Italy, the papilloma virus vaccine is distributed free of charge to girls under the age of 12; the most popular vaccines are cervarix (which offers protection only from HPV 16 and 18), gardasil, gardasil-9 and silgard. The vaccine is administered in three divided doses, and injected intramuscularly; the second dose is taken two months after the first, and the third after 4 months from the second.
In addition to the vaccine prophylaxis, it is possible to undergo post-contagion vaccination: after a presumed exposure to the virus, the woman can request the vaccine, a drug useful for treating the disease when the pathogen has already penetrated the body.
Even after vaccination, it is recommended - especially women - to continue regular routine checks: in fact, the vaccine does NOT protect against ALL types of Papilloma Virus.