Lichen puber planus
Lichen ruber planus represents a frequent morbid condition of the skin and mucous membranes, which consists of itchy papules, atrophic or erosive bubbles. Although it is hypothesized that the pathogenesis of lichen ruber planus is immunological, the etiology is still uncertain and unknown: in any case, it seems established that viruses do not affect in any way the manifestation of dermatosis.
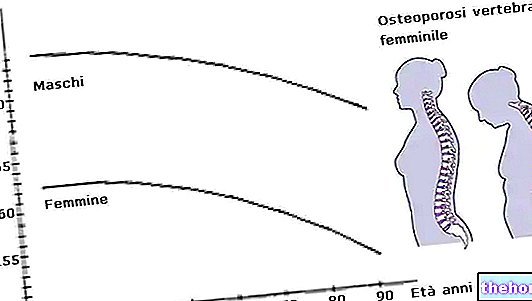
Incidence

Causes and affected areas
The triggering factors underlying lichen ruber planus are completely unknown: it has been found that sufferers of this dermatosis have strong states of anxiety, but the reason that regulates everything still remains a shadow area. Some authors venture a particular theory: based on the studies carried out, it seems that stress has a significant impact on the clinical evolution of the disease. The chronic course of lichen ruber planus, although benign, could therefore be fomented (not caused) by stress neurotransmitters [ taken from www.latuapelle.org].
Although it can ideally spread to all areas of the body, lichen ruber planus mainly affects the wrists, the lumbo-sacral area, the hips and the genitals; furthermore, nails, oral and genital mucous membranes, and scalp are also possible targets of dermatosis.
Injuries
It is difficult to construct a clear clinical picture, since lichen ruber planus does not manifest itself with the same skin lesions in every patient: the typical papules of the disease can be different in shape, size, location and arrangement, sometimes making recognition of the disease difficult.
Statistical data reveal that in 10% of cases the whitish papules of lichen ruben planus tend to heal in the central area, but to expand towards the periphery, with a particular circular trend (typical manifestation of lichen at the glans level, sometimes responsible for balanoposthitis or balanitis). Rarely, lesions follow a linear distribution.
- Localization of lesions
The papules in the skin take on a polygonal appearance, reddish or whitish, with a diameter that can vary from 3 to 10 mm. On the internal mucous membranes of the cheeks (mucous genes) and on the tongue, on the other hand, lichen ruber planus could favor the formation of branched and reticulated whitish papules. Furthermore, lichen ruber planus at the palmar-plantar level could generate rigid and hyperkeratotic reliefs, very similar to calluses.
The papules generated by lichen ruber planus can be located near the hair follicles, causing hair loss, with subsequent permanent damage to the follicle itself.
- Structure of the papules
In general, the papules of lichen ruber planus appear very small, comparable to the size of the head of a pin; but there are certainly exceptions, as these could increase in volume, spreading to the surrounding areas. When the papules no longer appear flat (hence the term "planus" of the disease), one speaks more correctly of lichen ruber acumunatus (a disease described for the first time around the mid-nineteenth century by MK Kaposi, a famous Hungarian dermatologist of the time ) today known as pithriasis rubra pilaris.
At the level of the limbs, the papules can take on a holed appearance, associated with the formation of particularly itchy warts.
A whitish reticulum appears on the papules of lichen ruber planus: it is a typical sign of dermatosis, which allows immediate recognition. The papules can remain isolated or group together forming real abnormal clusters. The main problem, which hinders the diagnosis, is given by the consistent scratching generated by the papules: the affected subject, through rubbing, removes the superficial film of the lesion, preventing clinical recognition.
In some subjects, the actinic type lichen ruber planus forms papules and bubbles, favored even more by sun exposure; in this form of lichen, the itching is almost nil.
Classification
Lichen ruber planus is classified according to the morphological characteristics of the papules and their location:
- Lichen ruber planus of the verrucous or hypertrophic type: typical lichen of the leg, in which the papules, dry and scaly, tend to be slightly raised from the skin. Often, papillomatosis (a pathology that is distinguished by the presence of papillomas at the cutaneous / mucous level) and evident hyperkeratosis are found.
- Bullous type lichen ruber planus: as the morbid condition foretells, blisters or bubbles of various sizes can form on the skin. The lesions are responsible for a progressive skin degeneration that damages the epidermal basal layer.
- Lichen ruber planus of the follicular type: dermatosis affects the follicles, creating considerable damage when the scalp is also affected, as it causes hair loss, therefore permanent non-reversible alopecia.
[taken from Treatise on clinical pathological anatomy by M. Raso]
Course of the disease
The disease can have a chronic or acute course, but fortunately it tends to regress spontaneously, without particular need for drug therapies (except for patients who complain of obsessive and relentless itching). When the formed plaques and papules change color, darkening, it is a clear sign of self-healing of lichen ruber planus.
Treatment
No case of asymptomatic lichen ruber planus has been reported: all patients complain of itching, although the intensity of the same can vary considerably from subject to subject. In some cases, itching is so negligible that drugs are not essential (lichen ruber planus of actinic type).
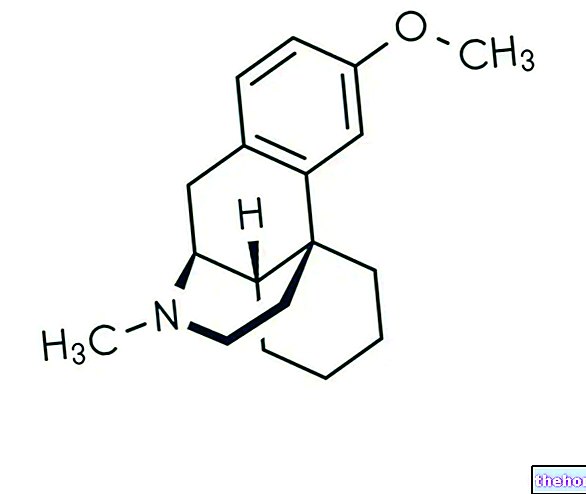
The patient, subject to medical prescription, can use creams or ointments based on corticosteroids (topical application) or oral administration of vitamin PP; the patient can also use antihistamines to soothe the itching.
When lichen ruber planus is accompanied by an evident anxious state of the patient, the administration of spasmolytic pharmacological specialties is recommended.
Summary
Lichen ruber planus: in short
Lichen ruber planus
Frequent morbid condition of the skin and mucous membranes, which consists of itchy papules, atrophic or erosive bubbles
- rather frequent disease among the fair sex
- incidence rate: around 1-2% of the healthy population
- the most affected subjects are aged between 30 and 60 years
It mainly affects the wrists, the lumbo-sacral area, the hips and the genitals. Lichen ruber planus is less common on the nails, oral and genital mucous membranes and scalp
Completely unknown
Stress and anxiety could foment the course of the disease
- It does not manifest itself with the same manifestations in all patients
- 10% of cases: Lichen ruber planus causes white patches that expand in a ring
- Linear lesions are rare
- Papule diameter: 3-10 mm, which in rare cases reach abnormal sizes
- Red (skin), white and reticulated papules (tongue, cheeks)
- Hyperkeratotic and rigid pads (palm)
- Pitted appearance of papules, associated with itchy warts (limbs)
- Permanent damage to the hair follicle
- Possible raised papules (lichen ruber acumunatus)
- Papules isolated or massed together
- Consistent itching that hinders immediate diagnosis
- lichen ruber planus of actinic type: favored by the sun. It does not itch
- Lichen ruber planus of the warty or hypertrophic type (leg)
- Bullous type lichen ruber planus (epidermal basal layer)
- Follicular type lichen ruber planus (follicles)
Chronic or acute course, but fortunately it tends to regress spontaneously
- corticosteroid creams or ointments;
- vitamin PP;
- antihistamines;
- spasmolytic drug specialties (when necessary).
Other articles on "Lichen Ruber Planus"
- Lichen Planus - Medicines for the treatment of Lichen Planus
- Lichen Planus
- Lichen Planus: therapeutic strategies