By binding to phosphorus (P), it first of all plays a "very important structural function (ratio 2.5: 1). The two salts, in fact, join and crystallize, forming l "hydroxyapatite. This "complex" mineral salt, deposited in an orderly way thanks to the orientation of some specific connective proteins (extracellular matrix), gives shape and structure to the bones, and therefore to the skeleton.
The western man introduces, in principle, quantities sufficient to satisfy his own needs; the latter, on the other hand, vary according to sex and age - they are greater in growth, old age - especially for women - gestation and breastfeeding.
While the excess of calcium, in physiological conditions, is not a problem thanks to the internal mechanisms of regulation, the chronic defect can favor complications and pathologies mainly affecting the skeleton (osteopenia, osteomalacia, osteoporosis).
The most abundant sources of calcium are of animal type (aged cheeses, milk, shellfish) - let's not forget, however, that phosphorus, of which milk and derivatives are rich, is its intestinal absorption competitor - but also vegetable foods contain levels of it. appreciable (especially legumes) - although the latter also bring anti-nutritional chelating elements such as oxalic acid.
and fabrics.
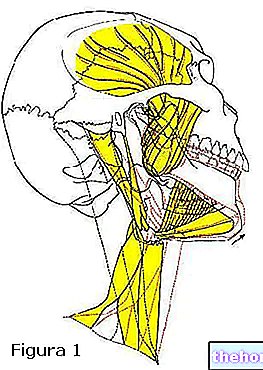
- It is vital for the health of the muscular, circulatory and digestive systems; for example, it regulates muscle contraction, nerve conduction and blood clotting;
- Together with phosphorus - with which it gives rise to hydroxyapatite - and mediated by hormonal factors such as vitamin D, it is essential for the construction of bone.
Note: approximately 98-99% of the total calcium is found in hydroxyapatite; in this way, the bones of the skeleton, in addition to being a real "scaffold" for the muscles, and a shield for the organs, act as a reserve It is therefore possible to deduce that calcium can be mobilized from the bone "reservoir" to meet some vital plasma and extracellular needs (metabolic priority).
- It supports the synthesis and function of blood cells (hematopoiesis).
Calcium inside the cells (intracellular calcium) intervenes:
- In the signal transduction pathways, where they act as a second messenger;
- In the release of neurotransmitters from neurons;
- In the contraction of all muscle cells;
- As cofactors in many enzymes;
- In fertilization.
The one outside the cells (extracellular calcium) is important for:
- Maintain membrane potential;
- Protein synthesis;
- Bone formation.
The hormones responsible for calcium metabolism are: parathyroid hormone, calcitriol (active form of vitamin D) and calcitonin.
(intake of vitamin D), partly to hormonal flows (see above: hormones responsible for calcium metabolism) and according to the age of the subject. The human intestine boasts the greatest potential for absorption in childhood and, gradually, this is reduced with aging, during which a significant reduction of 1,25 (OH) 2 cholecalciferol.
Calcium introduced from the diet is absorbed by two distinct ways:
- The first is saturable and occurs with an active transcellular transport mechanism; this process is mediated by a peptide vit. D-addict (Calcium Binding Protein) site in the outer membrane of enterocytes (intestinal mucosal cells) that binds calcium and transfers it to the basement membrane where it is released into the bloodstream by calcium-magnesium ATPase.
- The second way of absorption is passive diffusion, a process that is independent from the intervention of any hormonal factor.
Overall, calcium absorption is an extremely variable capacity, as it remains affected by:
- Calcium requirement of the subject;
- Presence of other molecules in the meal that affect the bioavailability of calcium:
- Increased by the presence of vit. D;
- Increased by the presence of sugars, especially lactose;
- Increased by the presence of the amino acids lysine and arginine;
- Increased by the presence of a basic intraluminal pH;
- Decreased by the presence of oxalates (anti-nutritional molecules);
- Decreased by the presence of phytates (anti-nutritional molecules);
- Decreased by the presence of phosphates;
- Decreased by the presence of nerves (caffeine, alcohol - anti-nutritional molecules);
- Decreased by the presence of uronic acids (of dietary fiber - anti-nutritional molecules);
- Decreased in conjunction with pathological malabsorption.