This condition is often associated with other inflammatory processes affecting the male genitourinary organs (including urethritis and prostatitis), although it can occur completely independently. In most cases, vesiculitis is usually caused by bacterial infections and can lead to infertility.
Manifestations of this condition include painful ejaculation, hematospermia, difficulty urinating (dysuria), increased daytime urination (pollakiuria), and sexual dysfunction (impotence or trouble maintaining an erection). These signals must act as an alarm bell and must induce the patient to promptly undergo an accurate clinical examination, which is also important to exclude any pathologies that occur with a similar symptomatological picture (including prostate cancer).
Treatment depends on the extent of the inflammation of the seminal vesicles and can include different pharmacological options (antibiotics, anti-inflammatory drugs, etc.) or surgical options, with the aim of improving the patient's symptoms.
; in this case, we speak more correctly of prostate-vesiculitis.
Seminal vesicles: what are they?
The seminal vesicles (or seminal vesicles) are two small structures, with a flattened conical shape, located along the course of the male genital tract. These even formations are found, one on each side, just above the prostate (posterior wall) and just below the urinary bladder.
To be clear, the prostate gland partially surrounds the first part of the urethra (duct that carries urine outside the body during urination), like a donut, at the neck of the bladder and merges with the two ejaculatory ducts that cross it.
What are the seminal vesicles used for?
The function of the seminal vesicles consists in the secretion of a viscous fluid, which constitutes a part of the ejaculate (about 70%). Combined with the seminal fluid produced by the prostate, this fluid helps to preserve the vitality of the spermatozoa.

The main constituent of the fluid produced by the seminal vesicles is, in fact, fructose, a sugar that represents the energy source of the spermatozoa, which come from the testicles, after passing through the epididymis and the vas deferens. The liquid produced by the vesicles also contains other substances such as: amino acids, prostaglandins, citrate and proteins.
Due to their location and the described relationships with neighboring organs, inflamed seminal vesicles can cause problems with urination and ejaculation.
, staphylococci and fecal bacteria (such as E. coli) coming from the intestine.
Favored by poor hygiene, inadequate immune defenses and behavioral factors (such as stress, smoking, alcohol, dietary imbalances and sedentary lifestyle), these bacteria can go up the urethra and reach the seminal vesicles. Often, this phenomenon also depends on sexual intercourse without the due precautions (such as unprotected oral sex).
At other times, the upwelling of pathogens results from problems with urine reflux or from the direct spread of bacteria from the urinary or genital tract to the urethra. More rarely, the infectious agents responsible for vesiculitis are transported to the prostate by blood or lymphatics from other organs in the body.
Non-infectious causes
Vesiculitis can also arise from non-infectious causes. In this case, it is not always possible to identify the exact reasons behind the inflammation of the seminal vesicles.
The combination of various predisposing factors may contribute to the onset of vesiculitis, such as:
- Stress and anxiety
- Immune disorders;
- Malformations of the urinary tract;
- Hemorrhoids;
- Professional or sports trauma;
- Sexual habits.
Furthermore, an important role is certainly to be attributed to the irritative stimulus due to:
- Incorrect diets;
- Excessive alcohol intake.
The risk factors favoring the onset of vesiculitis complete the picture:
- The recent insertion of a catheter into the bladder;
- The practice of intense efforts with a full bladder;
- Diabetes;
- Severe constipation;
- Prolonged sexual arousal without ejaculation;
- The practice of certain sports, such as cycling or horse riding.
Vesiculitis: types
From a clinical point of view, it is possible to distinguish the forms of vesiculitis into two large groups:
- Acute vesiculitis: it is often the result of a "bacterial infection; in these cases, the inflammation develops rapidly and has a rather short course, but the symptoms are quite intense and arise abruptly, suddenly."
- Chronic vesiculitis: it is characterized by continuous healing and relapses. In most cases, this type of chronic inflammation of the seminal vesicles is due to the implantation and proliferation of bacteria that resist antibiotic therapy.
To know
Acute forms of vesiculitis often result from neglected gonorrhea.
For further information: Gonorrhea - What is it? Causes and Symptoms (pollakiuria), painful (stranguria) and difficult (dysuria);
In addition, in case of acute vesiculitis there may be:
- High fever and chills (especially when the source of the inflammation is bacterial);
- Low back pain;
- General malaise;
- Groin pain.
In vesiculitis, the urine is often cloudy or has small amounts of blood (hematuria). Finally, perineal pain may be present, ie in the area between the anus and the base of the penis, and radiated differently from case to case (for example, towards the spermatic cord, testicle, urethra or thigh).
Vesiculitis can also involve disorders that affect the sexual sphere, such as:
- Blood in semen (hemospermia)
- Pain during intercourse or after ejaculation;
- Impotence or problems in erection (difficult or incomplete) and in its maintenance during coital intercourse;
- Frequent and painful nocturnal erections;
- Premature ejaculation.
In any case, these are often not very specific symptoms and similar to those caused by other diseases, such as bladder problems, urinary tract infections or prostatitis (inflammation of the prostate). These disorders can also be a sign of more serious conditions, such as prostate cancer. For this reason, it is always advisable to contact your doctor for the most appropriate tests for your case.
Chronic vesiculitis: how does it manifest itself?
In chronic vesiculitis, symptoms are milder than in the acute form, but they persist or recur repeatedly over a prolonged period, often more than three months.
Chronic vesiculitis manifests itself with various kinds of disorders, however more nuanced than the acute form and may include:
- Pain or burning when urinating
- Soreness of the perineal, suprapubic and inguinal area;
- Testicular discomfort
- Impairment of the general state of health.
If present, the fever is usually mild.
Vesiculitis: what are the possible consequences?
If continued over time, vesiculitis can cause infertility. At the analysis of the spermiogram and of the culture of the fluid produced by the seminal vesicles, the pictures that confirm this trend are characterized by:
- Leukospermia (presence of over 1 million white blood cells per ml in semen);
- Oligoastenospermia;
- Teratospermia;
- Agglutination of spermatozoa;
- Increased viscosity and pH.
Inflammation can be followed by sclerosis phenomena of the seminal vesicle wall and adhesions to nearby anatomical formations. The marked fibrous atrophy results in the progressive decrease in the quantity of seminal fluid in the ejaculate (secondary oligoposia).
In rare cases, vesiculitis evolves into a vesicular abscess which can result in peritonitis.
of the patient, asking him questions about the symptoms encountered, about the general health conditions, about the possible use of drugs, about sexual habits and so on.The history is followed by a complete examination, including digital rectal exploration, to palpate the seminal vesicles and evaluate their consistency through the anterior wall of the rectum. The diagnosis of vesiculitis is supported by the finding of swollen and very painful seminal vesicles.

What exams are useful?
An important role in the diagnosis of vesiculitis is played by urinalysis. In particular, urine culture is aimed at demonstrating the presence of signs of inflammation and identifying any responsible pathogens.
For the same purpose, the following can be performed:
- Seminal fluid analysis (sperm culture and spermiogram);
- Urethral swab.
Regarding blood tests, it must be considered that vesiculitis can cause a significant increase in PSA (Prostate Specific Antigen), especially if associated with concomitant prostatitis.
To define any urinary reflux problems, a simple uroflowmetry can be performed, which measures the speed of the urinary flow and the volume of urine emitted during urination, thus providing an "idea, albeit coarse, of any damage to the bladder."
To complete the clinical picture, a suprapubic vesico-prostatic ultrasound scan and, more rarely, trans-rectal ultrasound can be performed.
, although often, given the severity of the symptoms, the tests are postponed until after the resolution of the acute picture using broad-spectrum antibiotics.
After completing a course of antibiotics, another urinalysis will be performed to ascertain that the pathogen has been eradicated. If the test is positive for the presence of bacteria, an additional course of antibiotics will then be required.
To avoid relapses and phenomena of bacterial resistance, we remind you of the extreme importance of following the medical instructions to the letter, both as regards the doses and the treatment times.
Vesiculitis from other causes
Regarding the management of vesiculitis not sustained by an infection, the doctor may indicate the use of anti-inflammatory drugs and, to keep painful symptoms under control, analgesics. In addition, it is possible to resort to alpha-blocking drugs, useful for relax the prostate and bladder neck muscles, thus promoting better urine outflow.
During the treatment of vesiculitis, it is useful to adopt dietary changes, abolishing alcohol and irritants - such as hot spices, chocolate, coffee and artificial sweeteners - and trying to take adequate amounts of liquids and fibers, possibly supported by laxatives, if recommended by the doctor.
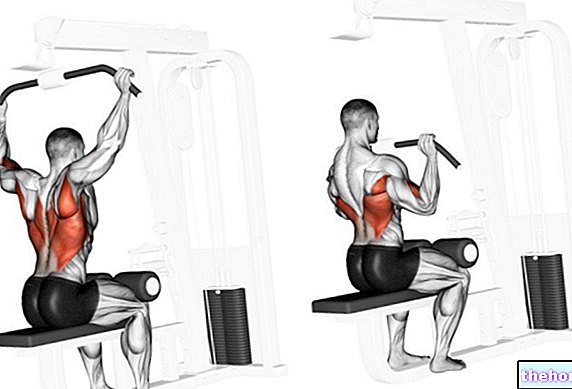
Until complete recovery, the patient should practice sexual abstinence and avoid physical activities that can cause perineal trauma, such as horse riding and cycling.
Surgery
In some cases, if the drugs are ineffective in resolving the vesiculitis and it is necessary to limit the patient's discomfort, a surgical approach may be considered, such as trans-urethral resection of the inflamed seminal vesicle (or both) or "removal with laparoscopy.