Generality
Mitral stenosis is a narrowing of the mitral, or mitral, valve of the heart. As a result of this narrowing, the disease compromises the regular blood flow passing through the orifice located between the left atrium and the left ventricle, controlled precisely by the mitral valve.

What is mitral stenosis. Pathological anatomy and pathophysiology
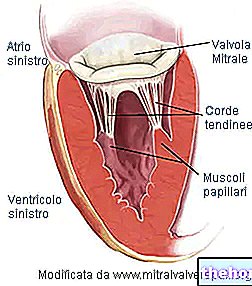
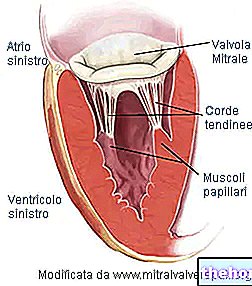
Mitral stenosis (from the Greek στενόω, narrow) is a narrowing of the mitral valve, such as to compromise its proper activity. The mitral valve is located at the orifice that connects the left atrium to the left ventricle of the heart. Its function is to regulate the unidirectional passage of blood, rich in oxygen, between the two cardiac cavities, during the phases of diastole and systole. In other words, in the heart of an individual with mitral stenosis, blood is impeded in its passage from the left atrium to the left ventricle.
Before examining how a mitral valve affected by stenosis looks and works, i.e. analyzing its pathological anatomy and pathophysiology respectively, it is useful to mention some fundamental characteristics of the valve:
- The valve ring. Circumferential structure that delimits the valve orifice.
- The valve orifice measures 30 mm in diameter and has a surface area of 4 cm2.
- Two flaps, front and back. For this reason, the valve is said to be bicuspid. Both flaps enter the valve ring and face the ventricular cavity. The anterior flap faces the aortic orifice; the posterior flap, on the other hand, faces the wall of the left ventricle. The flaps are composed of connective tissue, rich in elastic fibers and collagen.
To facilitate the closure of the orifice, the edges of the flaps have particular anatomical structures, called commissures. There are no direct controls, of a nervous or muscular type, on the flaps. Likewise, there is no vascularization.
- The papillary muscles. There are two of them and they are extensions of the ventricular muscles. They are supplied by the coronary arteries and give stability to the tendon cords.
- The tendon cords. They serve to join the valve flaps with the papillary muscles. As the rods of an umbrella prevent it from turning outward in strong winds, the tendon cords prevent the valve from being pushed into the atrium during ventricular systole.
Mitral stenosis results from a fusion of the commissures. The fusion can be more or less accentuated and transforms the orifice into a fissure. In cases of non-severe stenosis, or in the initial stage, the cusps may only appear thickened; vice versa, if the stenosis is severe, the flaps become rigid and there calcium salts are deposited (calcification).
The greater the narrowing of the orifice, the more severe the form of stenosis:
- Mild mitral stenosis, if the surface measures less than 4 cm2 but not less than 2
- Moderate mitral stenosis, if the surface measures between 2 and 1 cm2.
- Severe mitral stenosis, if the surface measures less than one cm2.
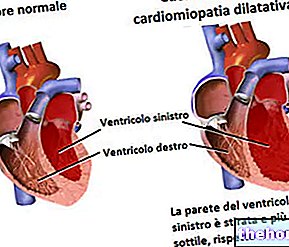
When normal blood flow through the mitral valve is obstructed, blood tends to accumulate in the atrium, the first cavity it passes through when it reaches the heart. This is oxygen-rich blood from the lungs. forced pause results in an increase in pressure inside the atrium and, in general, in everything upstream of the occlusion, including the lungs (atrial and pulmonary hypertension ensues). The situation reflects what happens to a a dam that continuously accumulates water and fails to discharge it. From the anatomical point of view, the increase in pressure determines a "hypertrophy of the walls of the" left atrium. Hypertrophy is an increase in the volume of cells. In this case, it is due to the increased effort that the cells make to push blood through a narrow orifice.
The accumulation of blood in the atrium, due to the reduction of the flow through the valve, and the consequent increase in pressure, generate a further change: the ventricular pressure, in fact, is lower than normal. This pressure is fundamental in the ventricular systole phase, that is, when the heart contracts to push blood into the vascular systems. If it is reduced, the range and flow of blood through the aorta also decrease. Thus, during a mitral stenosis, the following consequential events occur:
- The orifice of the mitral valve is narrowed.
- The blood stops forcibly in the left atrium.
- Atrial and pulmonary pressure increase
- The walls of the atrium become hypertrophic.
- Ventricular pressure is lower than normal because blood reaches the ventricle with greater difficulty.
- The blood output caused by ventricular systole is impaired.
- The flow of blood through the aorta is reduced.
Finally, two other anatomical aspects typical of mitral stenosis concern the left ventricle and the lungs. The left ventricle is deformed following a previous adaptation of the tendon cords and papillary muscles. This adaptation is created by the occlusion of the valve.
In the lungs, on the other hand, areas of edema are created, due to the stagnation of blood in the atrium and to the increase in pressure it produces in all the upstream vascular systems, especially in the pulmonary capillary system (pulmonary hypertension).
Causes of mitral stenosis
The main cause of mitral stenosis is due to rheumatic diseases.
The rheumatic origin of heart disease is attributable to a bacterial (streptococcal) infection of the airways. As a rule, following an infection, the human body responds with the production of antibodies, which kill bacteria, without complications. In some subjects, however, the antibody defenses produced against streptococcus also recognize the valve cells as foreign and attack them. Thus, an inflammatory state is created, which leads to deformation of the mitral valve. The latter is thickened and with cusps. merged with each other.
Other causes of mitral stenosis are:
- Senile degeneration, due to the progressive deposition of calcium salts (calcification) on the valve flaps. Calcification creates tissue stiffness. It is an event that leads to the 5th-6th decade of life.
- Congenital heart problems. Since birth, some structural elements of the valve are deformed.
- Valvular infections, due to endocarditis. An "endocarditis is a" bacterial infection typical of the internal cavities of the heart.
Symptoms and signs
When mitral stenosis is mild, the affected individual has no particular symptoms or problems.
On the other hand, when the stenosis worsens, the first symptoms appear, linked to the physiopathological aspects described above: above all, the increased pressure in the left atrium and in the upstream compartments prevails, including the lung. Therefore, the main symptoms are:
- Pulmonary and atrial hypertension.
- Dyspnea from exertion.
- Atrial fibrillation.
- Respiratory infections.
- Hemophtoe.
- Organic weakness, defined adynamy.
- Chest pain, due to angina pectoris.
Exercise dyspnea is difficulty breathing. In the specific case, it arises as a result of the lower outflow of blood towards the left ventricle and, subsequently, towards the aorta. The heart struggles to pump blood through the occluded mitral valve and the body's response to the consequent lack of oxygen consists in "increase the number of respiratory acts; respiratory acts that increasingly engage the heart. Furthermore, since the circulatory flow is obstructed in the left atrium, there is an accumulation of blood in all the upstream districts, including the pulmonary veins and lungs. This stagnation causes serious consequences: an "increased pulmonary pressure (pulmonary hypertension), the compression of the respiratory tract and, in the most serious cases, the leakage of fluids from the vessels to the alveoli. This last condition is the prelude to" pulmonary edema: in under such conditions, the oxygen-carbon dioxide exchange between alveoli and blood is compromised.
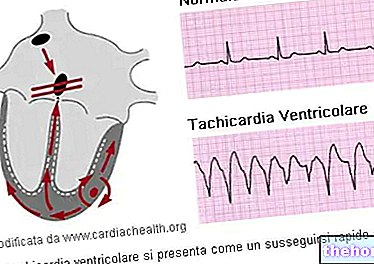
Atrial fibrillation is a "cardiac arrhythmia, that is, an alteration of the normal heartbeat rhythm." It is due to a disorder of the nerve impulse coming from the sinoatrial node. It results in fragmentary and hemodynamically ineffective atrial contractions (ie they do not ensure adequate blood flow). In fact, the left atrium is malfunctioning and the flow of blood, which flows into the underlying ventricle, is less than normal. It follows that even the ventricular contraction, which serves to push the blood into the aorta, is insufficient to meet the organism's demands for oxygen. Faced with this situation, the individual affected by atrial fibrillation increases the respiratory acts, manifests palpitation, pulse irregularity and, in some cases, fainting due to lack of air. The picture can further degenerate: the slowing of blood flow and the accumulation of blood in the vascular systems, especially if associated with an impaired coagulation, lead to formation of thrombus (solid, non-motile masses composed of platelets) inside the vessels. The blood clots can break down and release particles, called emboli, which, traveling through the vascular system, can reach the brain or heart. In these locations, they become an obstacle to the normal circulation and oxygenation of brain or cardiac tissues, causing the so-called ischemic stroke (cerebral or cardiac). In the case of the heart, it is also referred to as a heart attack.
Respiratory or thoracic infections are due to pulmonary edema.
Hemoftoe is the so-called blood spit, due to the rupture of the bronchial venules in the lungs. Again, pulmonary edema is the trigger.
Chest pain due to angina pectoris is a rare event. Angina pectoris is due to left atrial hypertrophy, ie of the left atrium. In fact, the hypertrophic myocardium needs more oxygen, but this demand may not be adequately supported by the coronary implant. It is therefore not a question of an "occlusion of the coronary vessels, but of an imbalance between the consumption and the supply of oxygen to the tissues.
The most characteristic physical signs, on the other hand, are:
- Mitral Facies.
- First and second tone, or snap, of opening the mitral.
- Diastolic murmur.
The mitral facies is manifested by a cyanosis of the face, especially of the lips.
The opening snap of the mitral is a noise, or tone, due to the sudden movement of the valve at the moment of the ventricular contraction of the heart. It is the consequence of the abnormal pressures inside the left atrial and ventricular cavities, as well as of the altered morphology of the valve cusps. This noise is attenuated when the mitral valve presents, on the flaps, calcifications, typical of advanced age.
The diastolic murmur is perceived when the mitral valve is open, in the diastolic or presystolic phase.
Diagnosis
Mitral stenosis can be detected by the following diagnostic tests:
- Stethoscopy.
- Electrocardiogram (ECG).
- Echocardiography.
- Chest x-ray.
- Cardiac catheterization.
Stethoscopy. The detection of a diastolic and presystolic murmur can be a clue to diagnosing mitral stenosis. The noise of a diastolic murmur occurs when blood passes through the stenotic mitral valve. It is perceived in the diastolic phase, since it is at this moment that the atrioventricular valves are open and the atrium has not yet contracted. The detection zone is in the 5th intercostal space, ie the one coinciding with the position of the mitral valve.
ECG. By measuring the electrical activity of the heart, the ECG shows hypertrophy, overload of the left atrium, and atrial fibrillation, all due to valve occlusion. Diagnosis by ECG gives an idea of the degree of severity of mitral stenosis: if the outcome is comparable to that of a healthy individual, it means that the stenosis is not severe; vice versa, the examination shows the three irregularities mentioned.
Echocardiography. Using the ultrasound emission, this diagnostic tool shows, in a non-invasive way, the fundamental elements of the heart: atria, ventricles, valves and surrounding structures. From echocardiography, the doctor can detect:
- Calcifications or rheumatic lesions of the elements that make up the mitral valve.
- Anomalies of the movement of the cusps.
- Increased size of the left atrium.
- Possible presence of thrombi in the left atrium.
- The maximum flow velocity, through the use of Doppler. From this measurement, it is possible to obtain the pressure values between the left atrium and the left ventricle.
Chest X-ray. It is useful for observing the situation in the lungs, verifying whether or not edema is present. Furthermore, it allows to see the increased volumes of the vessels upstream of the valve stenosis, due to hypertrophy and stagnation of blood.
Cardiac catheterization. It is an invasive hemodynamic technique. The purposes of this exam are as follows:
- Confirm the clinical diagnosis
- To evaluate in quantitative terms the haemodynamic alterations, that is of the blood flow in the heart vessels and cavities.
- Confidently define whether surgery can be performed.
- Evaluate the possible presence of other cardiac pathologies.
Therapy
Treatment depends on how severe the stricture is. A mild and asymptomatic stenosis, that is, one that has no symptoms, requires simple measures to avoid worsening:
- Clinical surveillance
- General hygiene rules to prevent bacterial infections, such as endocarditis.
If, on the other hand, the stenosis, even if slight, presents symptoms, the administration of some drugs is required:
- Digitalis, Beta-blockers and antiarrhythmics, in case of atrial fibrillation at the beginning.
- Diuretics, to reduce pulmonary hypertension.
- Anticoagulants, to prevent the formation of thrombi and emboli due to chronic atrial fibrillation.
- Antibiotics, when it is ascertained the presence of an "endocarditis, that is a" bacterial infection that afflicts the internal cavities of the heart. In this regard, it is good practice to recommend "careful oral and dental hygiene, to avoid predisposition to bacterial infections.
However, the therapeutic approach is different for individuals suffering from moderate or severe mitral stenosis. In this case, surgery is required. In particular, if the patient, after the appropriate diagnostic tests, presents with pulmonary hypertension and edema, the intervention becomes a priority.
The possible surgical operations are:
- Mitral Commissurotomy. The commissurotomy consists in the separation of the valve flaps, which have fused together following a rheumatic disease causing the stenosis. It is a real incision of the unnatural weld created. It can be performed using a balloon catheter - in this case we speak of percutaneous commissurotomy - or after a thoracotomy (open heart commissurotomy). This is not a valid approach for patients with cusp calcifications.
- Replacing the valve with a prosthesis. It is the most used intervention for the valves of those individuals affected by serious anatomical anomalies. A thoracotomy is performed and the patient is placed in extracorporeal circulation (CEC). Extracorporeal circulation is implemented through a biomedical device which consists in creating a cardio pathway. -pulmonary replacement of the natural one. In this way, the patient is guaranteed an artificial and temporary blood circulation that allows surgeons to interrupt the flow of blood in the heart, diverting it to another equally effective path; at the same time, it allows to operate freely on the valve apparatus. Prostheses can be mechanical or biological.
- Valvuloplasty. The stenosis is reduced with the use of balloon catheters, consequently regulating the altered atrial pressure and ensuring a better blood flow. It is indicated when mitral stenosis due to calcifications and stiffened flaps is ascertained. It is performed in a similar way to an angioplasty.
- Mitral valve repair. It is an approach indicated for stenosis due to a modification or a rupture of the tendon cords, which are replaced by the cardiac surgeon. It is also a valid solution in case of valve ring anomalies. Again, patients are placed in extracorporeal circulation.This method is not suitable for cases of mitral stenosis with rheumatic origin.