In most cases, HPV (acronym for Human Papilloma Virus) infections run completely asymptomatically, therefore without causing symptoms of any kind: the body's ability to eradicate the virus before it can cause major damage is extraordinary. even if unfortunately, in some circumstances, this ability fails and the immune system, while managing to stem and contain the infection, is unable to defeat the HPV, which thus causes symptoms and even quite serious disorders. Among the most feared, HPV infection can slowly transform a normal cell of the cervical epithelium (of the cervix) into a cancer cell; the key step in this process, which lasts at least a decade, is the integration of the viral DNA with the genome of the host cell.
HPV Symptoms
Most people (about 80%) infected with HPV overcome the infection within three years of infection without complaining of any particular symptoms or complaints.
Currently, over 120 HPV serotypes have been identified, each with its own unique biological and pathological characteristics; for this reason, each virus has been assigned an identification number (eg: HPV-1, HPV-2 ...).
Some HPVs are practically harmless to the body and do not cause particular disturbances or symptoms. About 40 types infect the genital mucous membranes and, among these, about 15 (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 ...) are defined as having a high oncogenic risk; in particular:
- Some HPVs are implicated in the onset of cervical cancer (also known as intraepithelial cancer of the uterine cervix): the strains most at risk are identified by numbers 16 (HPV 16) and 18 (HPV 18), which alone are responsible for 70% of cervical neoplasms; the same papillomaviruses are also responsible for neoplasms of the penis, anus, vagina, vulva and oropharynx, which from an epidemiological point of view are however of marginal importance compared to cervical cancer. Infections sustained by these viruses give rise to subclinical manifestations, not identifiable with the naked eye but appreciable through specific tests such as the pap test
About 1% of HPV positive women with high oncogenic risk develop a neoplasm of the uterine cervix; from the moment of infection to the onset of cervical cancer there is a latency period of several years, quantifiable in at least a decade. period, in general, the woman does not complain of any particular symptoms attributable to the papillomavirus, which is why the "identification of the early infection first, and then of the pre-neoplastic lesions, through pap-test and / or HPV DNA test allows doctors to intervene before the neoplasm manifests itself.
Symptoms of cervical cancer may be completely absent, or so mild and subtle that they go completely unnoticed. As cervical cancer progresses, and the chances of cure diminish, typical symptoms of the disease may appear. : bleeding after intercourse and slight pain during intercourse, watery or bloody vaginal discharge, sometimes with an unpleasant odor, pain in the pelvic region, vaginal bleeding outside the menstrual period or after menopause.
Other cancers related to HPV infection can also develop in the absence of signs or symptoms, typically only when they reach an advanced stage that is difficult to treat.
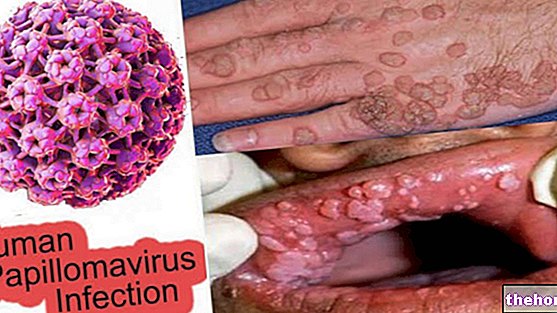
- Some HPVs are implicated in the onset of genital warts or sharp warts: the strains most at risk are identified by the numbers 6 (HPV 6) and 11 (HPV 11), responsible for the near thorality of cases; much more rarely the same HPVs are responsible recurrent respiratory papillomatosis, a condition characterized by the appearance of warts in the throat, with symptoms such as pharyngodynia, hoarse voice and difficulty in breathing Infections sustained by these viruses give rise to clinical manifestations, identifiable by the presence of particular signs and symptoms. Warts, in particular, can appear in the uterine cervix, vagina, vulva, urethra, perineum and anus, but also in extragenital sites: conjunctiva, nose, mouth, larynx. They often have such small dimensions that it is difficult to identify them with the naked eye.
- The strains responsible for genital warts are not the same ones involved in the onset of the aforementioned neoplasms; consequently a person affected by acuminate candyloma does not necessarily present an increased risk of anogenital neoplasms.
When symptomatic, the genital lesions - after an incubation time ranging from one to six months - appear as rough eruptions, more or less evident, confined to the genital area. In men, the warty growths infect, in particular, the glans, the urethral meatus, the frenulum, the shaft of the penis and the balano-preputial sulcus; in women, on the other hand, genital warts occur more frequently in the vulva, vagina and neck of the uterus. Fortunately, warty growths involve pain, irritation, itching and localized burning, of variable intensity, generally weak. Most of the time, genital warts are so small that they are not visible to the naked eye; other variants, on the other hand, can grow, aggregating and forming small groups of sharp warts, much more annoying.
Genital warts can also spread orally, in case of oral-genital sexual contact with infected partners or carriers.
See: Genital Warts Photos
We recall, to conclude, that some strains of papillomavirus (HPV 2 and HPV 4 in primis, but also HPV 1, 3, 26, 29,57 and others) are involved in the "onset of the so-called common warts, which typically occur at the level cutaneous, especially in the hands See: Photos Cutaneous Warts