Priapism is a pathological erection of the penis, not spontaneously reducible, often painful, prolonged beyond 4-6 hours, persistent even after any orgasm and in any case not necessarily related to sexual stimuli.
If not treated in good time, priapism - in addition to being rather annoying and embarrassing - causes permanent damage to the tissues of the penis, resulting in erectile dysfunction (impotence).

The term priapism derives from Priapus, Greek god of fertility, son of Aphrodite, endowed with a monstrously pronounced member in length and rigidity.
Symptoms and classification
The various forms of priapism are divided into two broad categories: ischemic or low-flow (venous priapism) and non-ischemic or high-flow (arterial priapism). The former, much more frequent, are characterized by the particular rigidity of the shaft of the penis (the glans, on the other hand, is typically soft), which is painful. In arterial priapism, on the other hand, the penis appears hot, erect but not too much rigid, therefore compressible and generally painless.
Patients with ischemic priapism can also develop intermittent forms, experiencing over time repeated erectile episodes interspersed with other detumescence episodes. This type of priapism mainly affects patients with haematological diseases.
Causes and consequences of priapism
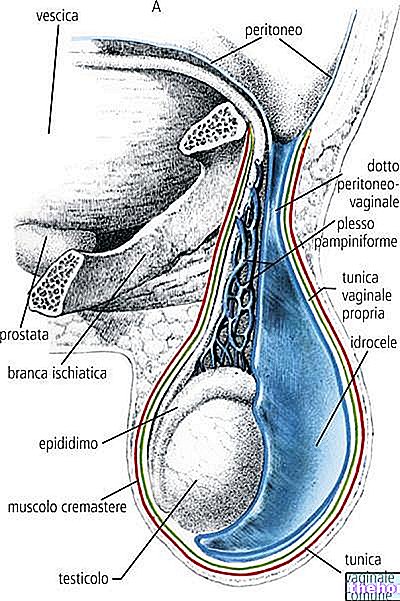
Priapism is a fairly rare condition, which more than real causal factors recognizes numerous, possible, predisposing elements. In most cases it is observed between 5 and 10 years and between the second and fifth decade of life; in childhood, the main cause is represented by sickle cell anemia, while in adulthood priapism is more often related to pharmacological causes. In most cases, moreover, the phenomenon occurs in the low flow form; as anticipated, in such circumstances we speak of venous priapism. In these cases, in fact, the prolonged erection is due to the lack of outflow of venous blood from the penis, with consequent haematic stagnation inside the corpora cavernosa. After a few hours, in the absence of a replacement blood, the smooth muscle cells begin to suffer from lack of oxygen; the state of local acidosis, with increased blood viscosity, and edema of the trabeculae, favors the maintenance of the state of priapism, hindering blood drainage. When anoxia becomes particularly prolonged, oxygen deficiency causes necrosis and fibrosis of muscle cells, resulting in permanent erectile deficit. For this reason, low-flow priapism - unlike arterial priapism - constitutes a "urological emergency, with a risk of complications that progressively increases over time.
Venous priapism can be caused by numerous systemic blood disorders, such as leukemia, sickle cell (or sickle cell) anemia, thalassemias, polycythemias, coagulopathies, haemophilia, dyserythropoiesis and thrombocytoasthenia. Other times neuromuscular factors come into play with alteration of the regulatory mechanisms of erection, systemic diseases (such as diabetes), but also neoplastic, infectious, allergic, toxicological (black widow's bite poisoning or scorpion sting) and pharmacological causes. to the latter, one of the most common causes of priapism in adults is linked to the intracavernous injection of erection-inducing drugs, such as papaverine, phentolamine or PGE1 (alprostadil). On the other hand, episodes of priapism linked to the abuse of new generation drugs, such as sildenafil, tadalafil and vardenafil, appear to be rarer. Other drugs that can favor the onset of priapism include the antidepressants fluoxetine and bupropion; drugs used against psychotic disorders, such as risperidone and olanzapine, active ingredients against anxiety, such as diazepam; anticoagulants such as warfarin (Coumadin) and heparin. Finally, we must not forget that priapism can also be triggered by alcoholism and the abuse of drugs such as cocaine, marijuana and ecstasis.
High flow priapism is less common than ischemic priapism and is linked to an increase in arterial flow in the corpora cavernosa, not sufficiently cleared by the normal venous outflow routes. In most cases it is caused by a genito-perineal trauma, which can damage a branch of the cavernous artery creating an arteriovenous fistula (direct pathological communication between veins and arteries). By virtue of the rich oxygenation of arterial blood, in these cases there is no impact on the erectile capacity of the penis.
What to do in the presence of priapism
In the presence of low-flow priapism, a rapid therapeutic intervention must be instituted to control pain and prevent erectile dysfunction secondary to fibrosis of the corpora cavernosa. A very important step is the diagnosis and correct identification of the causes of origin. to then prevent the occurrence of relapses. In the case of low-flow priapism, however, it is good to focus first on correcting the venous drainage.
Less aggressive therapeutic strategies resolve most cases of priapism; it is therefore recommended to start with these. The emergency treatment of venous priapism, therefore, first of all involves the aspiration of blood from the corpora cavernosa with or without irrigation of non-heparinized saline. In case of failure of the previous surgery, intracavernous injection of sympathomimetics is carried out by injecting vasoconstricting substances into the corpora cavernosa of the penis, such as phenylephrine, norepinephrine, etylephrine, epinephrine and metaraminol. In this regard, it is necessary to pay attention to the systemic effects linked to the possible entry into the circulation of these substances. Even ice, applied to a cloth to avoid burns, exerts a "vasoconstrictive action by increasing the sympathetic tone, thus stimulating the contraction of muscle cells. smooth vascular; however, as illustrated in the article, in the face of an episode of priapism it is advisable to go immediately to the emergency room to avoid permanent injuries.
The gradual transition from NSAIDs to opioids is indicated for the treatment of pain.
Before opting for a surgical solution, it is good to repeat the intracavernous injection procedure of sympathomimetics several times. In patients in whom the priapic picture does not resolve with medical therapy, an artificial veno-cavernous or cavernous-cancellous shunt can be performed to determine penine detumescence in order to bypass the venous occlusion, draining the blood into another vein. through an artificial fistula.
In cases of low-flow priapism, selective embolization of the arteries responsible for the fistulous passage (occluded through the use of various substances) has now become the treatment of first choice. The procedures described for the treatment of venous priapism are not indicated. , both because they are ineffective and because the high venous drainage would lead to the systemic diffusion of locally injected drugs, with possible relevant side effects. Furthermore, arterial priapism does not represent a "medical emergency and it is therefore good to wait for the results of the diagnostic tests.




.jpg)


















