Some sources distinguish two types of circumcision, based on the total or partial removal of the foreskin (thus leaving the glans partially uncovered). In reality, this distinction is not entirely correct, since circumcision is only one and concerns the removal total of the foreskin. The excision of a part of the preputial sheet is more precisely called postectomy.
From the ancient paintings, it is clear that the circumcision procedure dates back to at least 6,000 years ago, a very widespread practice especially in Egypt: still today, circumcision remains one of the most discussed methods in the medical field.

In the USA, it is estimated that the circumcision rate has decreased sharply (by about 90%) in recent decades, unlike the Korean countries, where circumcision was practiced mainly during the period of the Second World War.
Globally, it is estimated that approximately 13 million men undergo circumcision every year.
; micro-leaks of urine and smegma cannot stagnate between the foreskin and the glans, because they are considered risk factors for balanitis, postiti, balanoposthitis and other inflammations at the genital level.
Others undergo circumcision because they are driven by the desire to improve genital aesthetics or by the desire to perceive greater arousal during the sexual act.
Despite against their will, many men are forced to undergo circumcision, to resolve genital anatomical disorders (phimosis, paraphimosis) or for the treatment of premature ejaculation. urethra), urethral stricture, chronic penile lymphedema (rare). In some cases, penile cancer could also be cured, completely or partially, by circumcision.
Even the patient who wants to undergo circumcision for various extra-pathological reasons (religion, hygiene, etc.) must still go to the specialist, who will inform him of the procedure.
The surgical practice is performed in day-hospital: the patient is anesthetized in situ by inoculating 1% xylocaine (or lidocaine) directly into the nerves of the penis.
In the child, general anesthesia is preferable.
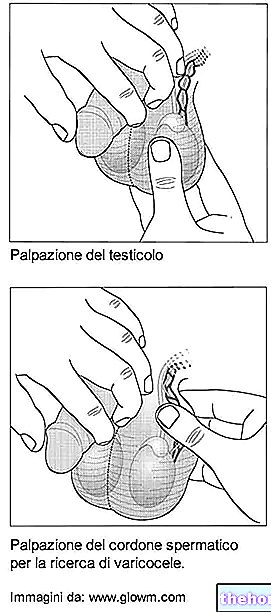
After having anesthetized the part of the patient, we proceed with the surgical removal of the flap of skin that covers the glans, using a laser or scalpel: the operation lasts approximately 40 minutes.
We recommend suspension from sporting activity for 7 days and sexual activity for about four weeks, to allow the wounds to heal definitively.
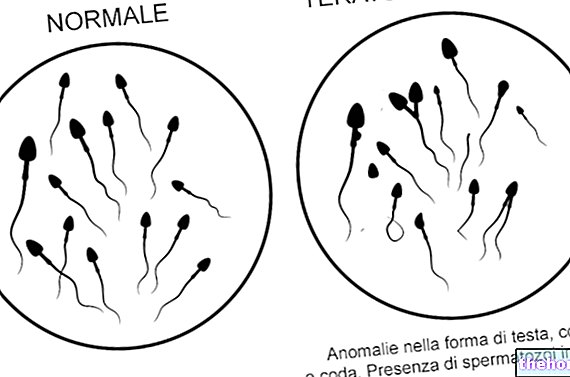
The stitches fall off spontaneously, usually after a couple of weeks; the reduction of sensitivity in the glans, with relative thickening of the aforementioned area, usually occurs after four weeks.
The patient is satisfied with the intervention in 80% of cases.

- Real circumcision: surgical removal of the foreskin covering the glans penis
- Glandular neurotomy: some nerve fibers located in specific points, near the sulcus of the glans, are dissected. In this way, the sensitivity at the glandular level is markedly decreased
Let's see, therefore, the reasons.
First of all, the foreskin seems to be the ideal habitat of the HIV virus: the anatomical area of the foreskin has all the ideal characteristics for the nesting of the virus, consequently through the removal of the part, the virus does not find the ideal conditions to settle .
Statistical data confirm the theory:
- 30% decrease in HIV / AIDS infections in women with circumcised partners (study carried out in Uganda, examining a sample of 12,000 people)
- Women with circumcised partners are less likely to get bacterial vaginitis and Trichomonas vaginalis
- Reduction of AIDS patients in African regions where circumcision is a very widespread practice
It should be pointed out that male circumcision is not used as a prophylaxis against chlamydia, syphilis and gonorrhea. Regarding the possibility of decreasing the risk of HPV (papilloma virus) following circumcision, there are conflicting theses: some believe that circumcision is not a prophylactic practice against HPV, other research exponents, however, are more hopeful. Therefore, it is not yet possible to state with certainty that HPV can be prevented through male circumcision: it will take a few more years for these hypotheses to be confirmed or not.
However, condoms remain the safest method of protection from STDs.
Circumcision: Complications and Reflections






.jpg)


















