Definition of cryptorchidism
Cryptorchidism designates a very frequent pathological picture among infants: it identifies the failure of one or both testicles to descend into the scrotal bursa, since they are believed to be in the inguinal canal or inside the abdominal cavity (rarer case), even before development. As can be guessed, cryptorchidism is a pathological condition that attracts the attention of many pediatricians, urologists, geneticists and oncologists, both for the complexity of the condition itself, both for the consequences that the disease could generate in adulthood. Despite what has been stated, cryptorchidism does not seem to represent an important object of study, given the scarce longitudinal studies carried out on cryptorchid subjects, from infancy to adulthood.
Term analysis
As for the vast majority of medical terms, cryptorchidism also derives from the Greek: the root crypto- κρυπτος (hidden) and the ending όρχυς (testicle) perfectly anticipate the disease.

Incidence
In the light of what emerges from medical statistics, it seems that cryptorchidism is the most frequent anomaly affecting the urogenital tract of infants and infants. Furthermore, it is not uncommon for cryptorchidism to occur especially among preterm infants (incidence ranging from 9 to 30%); it is also estimated that the disease affects 3-5% of children born within the established term.
In 2000, it is assumed that those born with cryptorchidism were 15,000-30,000. In about half of the cases, cryptorchidism regresses spontaneously in the first or second year of the child's life; unfortunately, however, the number of children who do not heal naturally is increasing and, if they do not undergo surgical therapy, they are destined to remain cryptorchids for life. [taken from Cryptorchidism: pathophysiology, clinic, medical and surgical therapy by C. Spinelli].
Furthermore, it appears that cryptorchidism is unilateral in 60-65% of cases (failure to descend only one testicle, especially the right one), and bilateral in 30-35% (involving both testicles).
The incidence of the disease seems to have increased considerably in recent years: pollution and changes in estrogen are attributable.
Embryogenesis
To understand the real reason that causes cryptorchidism, it is necessary to take a step back and talk about embryogenesis. The mechanisms that regulate embryonic genesis are very complex, so below is a simplistic summary of the localization of the testicles in physiological conditions, during Development:
- 1st - 8th week: differentiation of the testicles in the upper lumbar area;
- 8th - 12th week (third month): beginning of the migration of the testicles towards the scrotum (sac in which the testicles are enclosed);
- 3rd month - 7th month: the testicles reach the deep inguinal ring, and then reach the inguinal canal;
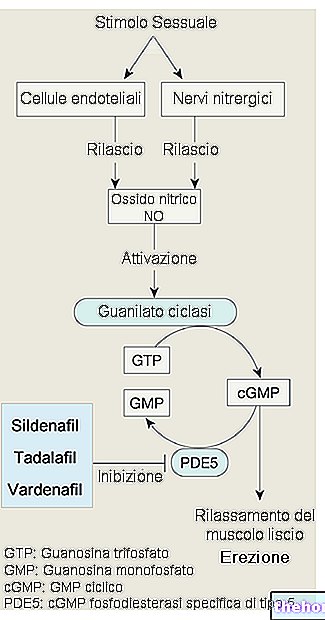
- 9th month: the testicles are located inside the scrotal sac, thanks to the stimulus given by gonadotropins and androgens (not surprisingly, to treat cryptorchidism pharmacologically, these types of hormones are administered). [Taken from Genetics in Male Infertility by Salvatore Raimondo, Valerio Ventruto, Andrea Di Luccio]
Classification
Cryptorchidism is differentiated on the basis of the location of the testicle (s) during the descent: the cryptorchid testicles, in fact, can be located in the abdominal area (high or low), in the groin area or near the suprascrotal or scrotal site high.
Contrary to what one might think, acquired cryptorchidism exists, although it is a rather rare form: generally, in such situations, the descent of the testicle can be the consequence of an "inguinal hernia.
When the testicles are completely absent in the patient, we no longer speak of cryptorchidism, but of real anorchia.
Based on the location of the testicle, cryptorchidism is distinguished into:
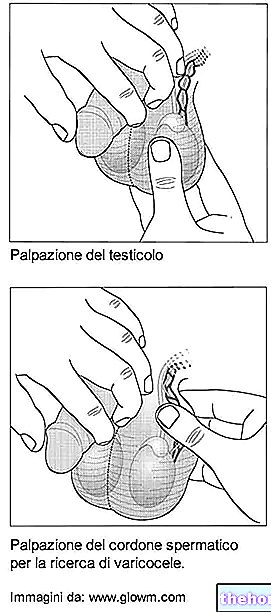
- true cryptorchidism (undescended testicle): medical palpation of the testicle is denied, as it is located near the abdominal cavity;
- ectopic cryptorchidism: as previously analyzed, the testicle is located in an anomalous region, outside the sites normally traveled during the descent;
- cryptorchidism with retractable testicle: occasionally, the testicle returns to the inside of the scrotal bag: no surgical or pharmacological treatments are essential, considering that the testicle can be repositioned inside the scrotal bag through rather simple manual maneuvers;
- cryptorchidism with incomplete descent of the testicle: the testicle is "blocked" at the level of the inguinal canal or of the external inguinal orifice (areas that the testicles travel through during the embryonic stage).
[taken from www.andrologia.it]
In the various types of cryptorchidism, the testicle can be palpable or not palpable: this last case represents the least frequent form (8%). The non-palpable testicle usually occurs in agnesia, where it is localized in the abdomen or in the inguinal canal; the endo-abdominal testicle is not palpable manually nor detectable with ultrasound along the descending path of the gonad (usually video-laparoscopy or surgical exploration is used).
[adapted from Cryptorchidism: pathophysiology, clinic, medical and surgical therapy by C. Spinelli].
Other articles on "Cryptorchidism"
- Cryptorchidism: causes and complications
- Cryptorchidism: symptoms, diagnosis, therapies
- Cryptorchidism: summary table













.jpg)











