Generality
Graves' disease is the most common cause of hyperthyroidism worldwide, with an average incidence that - although subject to wide geographical variations - is between 1.5 and 3% of the population.
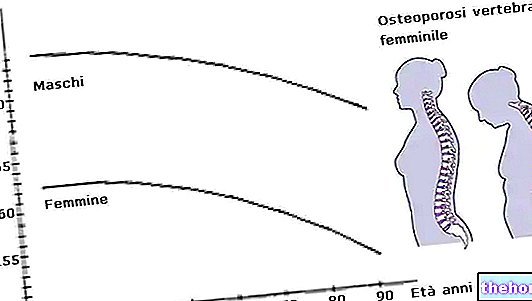
Also known as Graves 'disease or diffuse toxic goiter (given the uniform increase in thyroid volume, with the absence of nodular formations), Graves' disease prefers mainly women, with a male / female ratio of 1: 5-10.

Symptoms
For further information: Graves' disease symptoms
The onset of the disease may be accompanied by rather vague symptoms, with difficulty in recognizing their nature in the immediacy.The first to appear are above all mental disorders, which are maintained even in the full-blown phase of Basedow's disease; the patient can thus complain of anxiety, difficulty falling asleep, excessive emotionality, irritability, restlessness, easy worry for irrelevant or completely absent reasons, depression, disturbances of ideation, tremors and easy mental fatigue.
In the full-blown picture, Graves' disease is accompanied by the other typical symptoms of thyrotoxicosis: tachycardia, arrhythmias (up to atrial fibrillation), weakness, heat intolerance with copious sweating, episodes of redness of the face and neck, menstrual disorders up to " amenorrhea, decreased libido and fertility, alvus disorders with frequent diarrheal episodes, increased thyroid volume (goiter), shortness of breath, onycholysis (fragility of the nails with a tendency to fixate), hand tremors with rapid, fine and irregular oscillations , and weight loss despite hyperphagia, which in some cases can lead to weight gain (Basedow fat).
Typical of Graves' disease is also the so-called exophthalmos, a condition in which the eyes protrude outwards, becoming protruding and fixed until they give the face - in an advanced stage and in the absence of treatment - a "spirited" appearance. early oculars, which precede the actual exophthalmos, are limited to increased lacrimation, with photophobia, corneal and / or conjunctival irritation, and a sensation of sand in the eyes.

The neck of the patient with Graves' disease may have a swelling in the anterior region due to goiter (uniform but not always present increase in the thyroid gland).
Many of these symptoms may remain vague in the elderly patient, except for asthenic, cardiovascular and myopathic ones, which tend to accentuate instead. Furthermore, the history of the disease does not generally have a uniform course, but is characterized by the alternation of remissions and relapses, sometimes particularly intense (thyrotoxic crisis or storm).
Causes
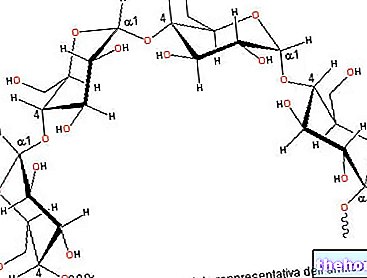
While remaining unknown in many respects, the origin of Graves' disease is essentially autoimmune based and is influenced by an important genetic and hereditary component. In fact, in patients' serum it is possible to find abnormal antibodies directed mainly against the TSH receptor (pituitary hormone that stimulates the synthesis of thyroid hormones); the chronic binding of these antibodies to the TSH receptor traces the stimulatory effects of the hormone on glandular activity. The result is a thyrotoxicosis due to functional hyperactivation of the thyroid, with an increase in the circulation of both thyroid hormones (FT4 and FT3) and blockage of TSH (almost always undesirable given the known negative feedback effect exerted by thyroid hormones). Still rather obscure remains the reason for this antibody attack.
Diagnosis
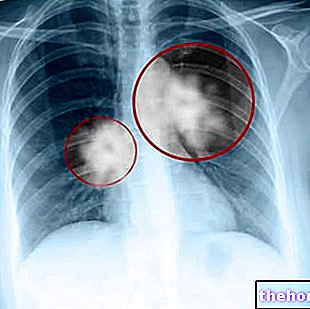
To diagnose Graves' disease, in addition to the "clinical examination of the patient (search for the symptoms and risk factors listed above), the dosage of thyroid hormones, TSH and antithyroid antibodies, associated with ultrasound images of the thyroid with echocolordoppler. (to investigate the vascularization.) Unlike in the past, the scintigraphic examination is not normally required.
Treatment
See also: Drugs for the treatment of Graves-Basedow's disease
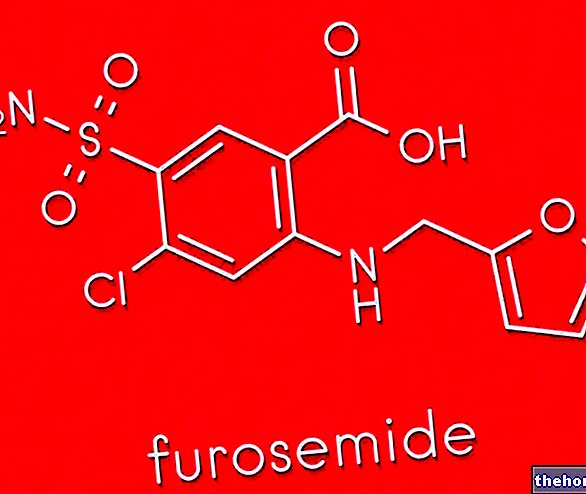
Basedow's disease therapy aims to reduce the amount of circulating thyroid hormones and to this end makes use of thyrostatic drugs, thionamides, with immunosuppressive action. These drugs are represented by methimazole, propylthiouracil (preferred in pregnancy) and, secondly, lithium carbonate and propranolol.
Pharmacological therapy of Graves' disease must be continued at gradually decreasing doses and - with a dosage calibrated on the individual patient based on the aggressiveness of the disease - continued until clinical hormonal remission of the hyperthyroid syndrome (6-24 months). When the drug treatment does not produce the desired results or must be interrupted for too many side effects (excessive reduction of the blood count of white blood cells, with alarm symptoms such as sore throat and fever), the doctor may decide to surgically remove good part of the thyroid gland or treat it with radioactive iodine (in both cases there is a risk of chronic hypothyroidism and relapse). The treatment of Graves' disease exophthalmopathy deserves a separate discussion, which makes use of ocular lubricants, local or systemic cortisone, radiotherapy of the orbit, up to various types of corrective surgery.