However, it is undeniable that menstruation has always represented an event that goes far beyond the simple reproductive function. For this reason it is good to know, at least summarily, the biological bases and thus avoid feeding all the unfounded beliefs at the basis of taboos that are in some ways still current.
it is an organ, exclusive to women, responsible for the production and maturation of female reproductive cells, called oocytes or egg cells; it is also important for the production of sex hormones.
Egg cells are produced exclusively during fetal life, surrounded by cellular structures called follicles; after birth, they partly regress and partly remain dormant until puberty. From this moment on, approximately every 28 days, a single follicle is brought to maturity, thanks to the intervention of the hormones produced by the hypothalamus and the pituitary (which are activated in an important way during puberty).
When the development phase is complete, the follicle explodes, letting out the egg cell (ovulation) which at this point can be, at least theoretically, fertilized.
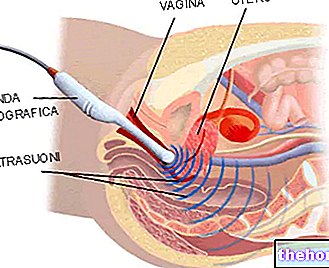
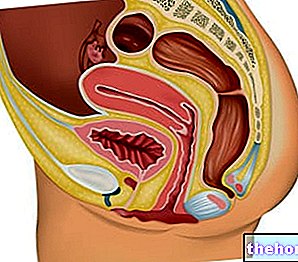
After liberation, the egg travels through the fallopian tubes and then enters the uterus; if during this process a spermatozoon enters it, which has risen through the vagina and the uterus after sexual intercourse, the egg cell is fertilized and the pregnancy begins.
To prepare for this eventuality, the organism implements a series of physiological modifications, first of all the increase in thickness of the endometrium; other transformations follow one another after ovulation, thanks to the intervention of the corpus luteum (a small structure that form in the ovary by transformation of the follicle after the release of the egg cell). If before ovulation these changes have above all the purpose of favoring fertilization (ensuring greater survival of the spermatozoa), the transformations induced by the corpus luteum have a different purpose. In this phase, in fact, the purpose is no longer to favor the fertilization, but to stimulate nesting.
This term, also known as implantation, indicates the complete and progressive penetration of the fertilized egg into the mucous membrane that lines the uterine cavity (called the endometrium). This phase, which begins 5 or 6 days after fertilization, is favored by endometrial glands, whose secretory activity is stimulated by hormones (progesterone) secreted by the corpus luteum.
If the egg cell does not meet spermatozoa during its journey, it undergoes a spontaneous regression within 12-24 hours; within about ten days the corpus luteum also ceases its endocrine production and regresses, forming a very small scar on the ovarian surface. The modifications of the endometrium no longer have any reason to exist and the alteration of hormonal levels leads to the flaking of its external surface, giving rise to menstruation. Menstrual flow is therefore not made up exclusively of blood, but also of proteins, water, mucus and other cellular elements.
In the event that fertilization has not occurred, ovulation always precedes menstruation by about fourteen days, regardless of the length of the cycle; on the contrary, the first phase, which goes from the last menstruation to ovulation, is variable and can give rise to more or less long cycles of the four canonical weeks (21-35 days).
Immediately after menstruation, hypothalamic and pituitary hormones stimulate the maturation of a new follicle; the proliferation of the endometrium is reactivated and the body prepares for the umpteenth time for a possible pregnancy.
.
Most often, menstrual flows after the first are quite irregular, but they tend to stabilize within two years. For example, there is no need to worry if after the menarche the flow does not recur in the next 30 or 60 days.
If the menstrual flow does not appear by the age of 16, we speak of primary amenorrhea, a condition that can be linked to hypothalamic-pituitary lesions or, more frequently, to anatomical malformations (imperforation of the hymen, congenital malformations of the uterus or vagina, ovarian failure). Especially if the breasts and pubic hair have begun to grow, but menstruation has not yet appeared by the age of sixteen, a medical consultation is advisable: "amenorrhea could in fact be linked to a constitutional" delayed puberty ", but there it is also the risk that it may be an expression of pathological factors.
Curiosity
The prefix "men" - also common to other medical terms such as menopause, menorrhagia, etc. - derives from the name of Mena, daughter of Jupiter, goddess in charge of menstruation and fertility.
estroprogestiniche helps to regulate the duration of "menstruation" and to decrease the overall flow.in menstrual blood could indicate menorrhagia or uterine bleeding.
?read the dedicated article "Menstruation: Questions and Answers".
Further articles that may interest you are:
- Menstrual Cycle and Fertility
- Premenstrual syndrome
- Birth control pill
Menstruation, Pregnancy and Lactation
- Implant losses
- Menstruation and pregnancy
- Lootations and postpartum losses
- Menstruation and breastfeeding
Alterations of the Menstrual Cycle
- Dysmenorrhea - Menstrual pains
- Oligomenorrhea
- Hypomenorrhea
- Metrorrhagia
- Menorrhagia
- Painful ovulation - Mittelschmerz
- Spotting
- Hypermenorrhea
- Polymenorrhea
- Menstrual changes in premenopause
How to manage your period
- Menstrual Cups
- Internal absorbents
- Nutrition and Premenstrual Syndrome
- Remedies for Menstrual Pain
- Remedies for the Irregular Menstrual Cycle
- Premenstrual Syndrome Medications
- Painful Menstruation Medications