The calcaneus is one of the 7 bones of the tarsus; the tarsus is one of the three bone groups making up the skeleton of the foot.
Often associated with plantar fasciitis or problems with the Achilles tendon, the heel spur is the possible consequence of: injuries to a tendon or muscle of the foot, excessive strain of the plantar fascia or repeated tearing of the periosteum of the heel.
The most characteristic symptom of heel spurs is foot pain.
For a correct diagnosis, the most important examination is the x-ray of the foot.
First-line treatment is conservative; in case of failure of the latter, the alternative is surgery.

Brief anatomical reminder of the foot: localization of the calcaneus
Anatomists divide the bones of the foot into three groups: the tarsal (or tarsal group) bones, the metatarsal (or metatarsal group) bones, and the phalanges.
- Tarsal bones or of the tarsal group or of the tarsus. Located just below the ankle joint, there are a total of 7 irregularly shaped bony elements: the talus (or talus), the calcaneus, the navicular, the cuboid and the three cuneiforms (lateral, intermediate and medial).
- Metatarsal bones or of the metatarsal group or metatarsal. Belonging to the category of long bones, there are 5 elements in all, arranged parallel to each other. The proximal section borders on the cuneiform tarsal bones and the cuboid; the distal section, on the other hand, borders on the phalanges.
- The phalanges. There are a total of 14 and represent the bony elements making up the toes. Except the first finger - the only one made up of 2 phalanges - all the other fingers have 3 phalanges each.

they are small bone spurs, similar to a rose thorn, a beak or a claw, which form along the joint margins of bones subjected to chronic erosive and irritative processes.
TYPES OF CALCANEAR SPINE
There are two main types of heel spurs: the inferior heel spur and the posterior heel spur. As you can guess from the names of the two types, the element that distinguishes the two conditions is the localization of the osteophyte on the calcaneus.
- Inferior heel bone: the osteophyte resides on the sole of the foot, below the calcaneus, precisely at the level of the insertion point of the plantar fascia.
In most cases, this condition is associated with plantar fasciitis; more rarely, with ankylosing spondylitis. - Posterior calcaneal spine: The osteophyte resides in the posterior part of the calcaneus, at the level of the insertion of the Achilles tendon. Normally, it is also visible to the naked eye.
Most often, this condition is associated with an "inflammation of the Achilles tendon".
What is the plantar fascia?
The plantar fascia is a ligament, located on the lower edge of the foot (sole), which runs from the bones of the heel (calcaneus) to the bones of the toes. Morphologically similar to an arch, it allows the foot to be curved and acts as a cushion that absorbs the shocks of walking, running, etc.
Like any ligament, the plantar fascia is made up of connective-fibrous tissue.
The formation of osteophytes is a phenomenon of bone neo-apposition, triggered by erosive and irritative processes affecting the bone on which the anomaly appears.
In the case of the heel spur, the causes of the latter are generally injuries to a tendon or muscle of the foot, excessive stretching of the plantar fascia or repeated tearing of the periosteum of the heel (NB: the periosteum is the whitish membrane that covers the bone).
LESS COMMON CAUSES
More rarely, heel spurs can also be the result of inflammatory diseases, such as reactive arthritis, ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis.
RISK FACTORS
Risk factors for heel spurs include:
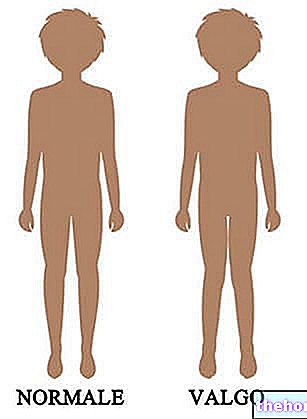
- Walking with an abnormal gait, which involves excessive stress on the calcaneus, the ligaments located near the calcaneus and / or the nerves running near the calcaneal bone;
- Running or jogging on very hard surfaces;
- Wearing unsuitable shoes, especially those that involve excessive modification of the foot arch;
- Being overweight or suffering from obesity.
RISK FACTORS OF CALCANEAR SPINE AND FOOT FASCITES
Since heel spurs are often associated with plantar fasciitis, it is worth remembering the risk factors for this second condition:
- Old age. Aging involves a reduction in the flexibility of the plantar fascia and a thinning of the fat pad located inferior to the calcaneus;
- Diabetes;
- Spending many hours of the day on your feet;
- Inadequate physical activity (ex: over-training, inadequate warm-up, etc.);
- Suffering from flat foot or pes cavus.
What is plantar fasciitis?
Plantar fasciitis is a very annoying injury to the plantar fascia.
Its presence causes pain in the heel and, sometimes, also in the central part of the foot and the forefoot.
Plantar fasciitis is often the result of a combination of contributing factors; rarely, in fact, is it the result of only one cause.
The heel spur can be asymptomatic - that is, it does not cause any disturbance - or symptomatic.
When symptomatic, the most common clinical manifestations consist of:
- Intermittent or chronic pain during walking, jogging or fast running activities. In the most severe cases the pain also appears when standing for many consecutive hours;
- Sense of soreness in the tissues surrounding the heel spur;
- Sense of pain in the tissues that reside around the heel spur.

SYMPTOMS OF CALCANEAR SPINE ASSOCIATED WITH PLANTAR FASCITIS
The symptom picture of when the heel spur is associated with plantar fasciitis includes:
- Pain, similar to a twinge, in the heel. The painful sensation is due to an inflammatory process affecting the plantar fascia;
- Pain in the sole of the foot, after long periods of standing, long walks, running activities etc;
- Foot pain in the morning. The presence of morning pain is a consequence of the shortening of the plantar fascia, which takes place during night rest, due to the position assumed by the toes. Upon awakening, the movements of the feet require an elongation of the plantar fascia and this involves, where the plantar fascia is injured, the appearance of an annoying painful sensation.
Intense morning pain is transient.
Foot x-rays provide sufficiently clear images of the bones of the foot and the abnormalities they may have. It is a painless procedure; however, it should be noted that, during its execution, the patient is exposed to a small dose of ionizing radiation which is harmful to the health of the human being.
DIAGNOSIS OF ASSOCIATED CONDITIONS
Physical examination and medical history are essential to diagnose possible conditions associated with heel spurs (eg plantar fasciitis, Achilles tendon problems, etc.).
The physical examination is the set of diagnostic maneuvers, carried out by the doctor, to verify the presence or absence, in the patient, of the signs indicative of an abnormal condition.
The anamnesis is the collection and critical study of the symptoms and facts of medical interest, reported by the patient.
CONSERVATIVE THERAPY
Conservative therapy does not allow to eliminate the heel spur, but still guarantees excellent results against painful symptoms.
The most common conservative treatments, which can be adopted in the case of heel spurs, consist of:
- A period of rest from all those activities that favor the onset of pain (eg: running, long walks, etc.);
- The administration of pain medication, to reduce the painful sensation. Examples of painkillers that can be administered are: paracetamol, ibuprofen and naproxen;
- Exercises of stretching (or muscle lengthening) and strengthening for all the muscles of the leg that refer to the Achilles tendon. This is useful both in the case of heel spurs associated with problems with the Achilles tendon, and in the case of heel spurs associated with plantar fasciitis ;
- The use of shoes that do not press on the heel spur;
- The use of plantar orthoses to be inserted in everyday footwear and not only. They are useful for reducing the painful sensation both in the presence of plantar fasciitis and in the presence of Achilles tendon problems;
- Physiotherapy exercises aimed at preventing plantar fasciitis and Achilles tendon disorders.
SURGICAL THERAPY
Surgical therapy for the heel spur includes the removal of the osteophyte and, for cases associated with plantar fasciitis, the plantar fascia distension surgery (NB: readers interested in this second surgical operation can consult the article present here ).
After surgical therapy, it is important that the patient follows the advice of the doctors, for an effective and uncomplicated recovery.
The medical advice includes: rest until complete recovery of the foot's functionality, the application of ice to relieve the intervention site, the elevation of the leg and the avoidance of immediately loading the operated foot (the "use of crutches).
Some possible complications of the surgical practice are: infections, neuropathic pain due to the lesion of some nerve endings, a sense of numbness in the foot and scars at the site of intervention.
As a rule, in the case of heel spurs, doctors consider surgical practice to be essential when conservative therapy has not been successful and when the symptoms persist incessantly for 9-12 months.