Generality
Myasthenia gravis is a chronic disease characterized by fatigue and weakness of some muscles. It is an autoimmune disease in which the normal transmission of contractile signals sent from the nerve to the muscle is compromised.

In pathogenesis, some autoantibodies block postsynaptic receptors in the neuromuscular junction and inhibit the excitatory effects of acetylcholine (neurotransmitter). By reducing the signal efficiency, the patient experiences weakness, especially when trying to repeatedly use the same muscle. Initial symptoms of the disease include drooping of the eyelids (ptosis), diplopia, difficulty speaking (dysarthria) and swallowing (dysphagia). Over time, myasthenia gravis affects other muscle areas; the involvement of the thoracic muscles leads to severe consequences on respiratory mechanics and, in some cases, patients have to resort to artificial respiration. The condition is extremely debilitating and sometimes even fatal. Current treatments for myasthenia gravis are aimed at dulling the immune system response by reducing blood levels of autoantibodies.Treatment may include acetylcholinesterase inhibitors or immunosuppressants, and, in selected cases, thymectomy (surgical removal of the thymus).
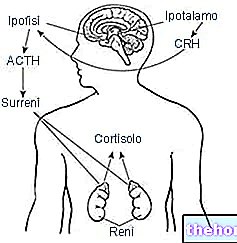
In short: how neuromuscular transmission occurs
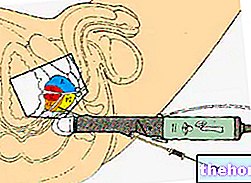
In a healthy neuromuscular junction, the signals generated by the nerves produce the release of acetylcholine (Ach). This neurotransmitter binds to the receptors (AChR) of muscle cells (at the endplate), causing an influx of sodium ions, which indirectly cause muscle contraction.
Causes
Communication between nerves and muscles Myasthenia gravis is an autoimmune disease. This means that it develops as a result of a "selective overactivity of the immune system, in which patients produce abnormal antibodies (Ab), because they are directed against a particular target in their body.
Normally, Abs are produced in the immune response against foreign agents such as bacteria or viruses. In myasthenia gravis, however, the immune system mistakenly attacks normal components of the body's tissues. Specifically, autoantibodies specific to the body's receptors are produced. acetylcholine (AChR), which bind to them and inactivate them. The end result is a drop in the number of free receptors expressed on the muscle cell surface. The loss of these surface receptors makes the muscle less sensitive to neuronal stimulation. Consequently, the "increase in autoantibody levels reduces the efficiency of the neuromuscular junction, so patients with myasthenia gravis show a progressive weakening of muscle tone." Vigorous physical activity requires an increase in chemical messages (with fewer available receptor sites, motor neurons are unable to reach the potential threshold to conduct the signal.) This helps explain why people with myasthenia gravis have worsening symptoms after physical exertion and feel better after rest. cause of this abnormal immune response is not yet fully understood.
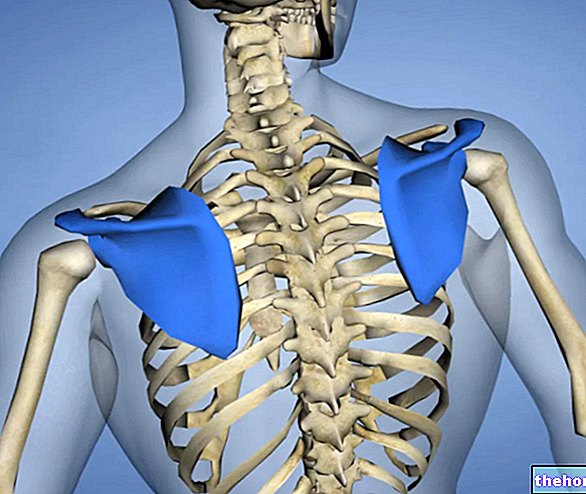
Thyme. In some people with myasthenia gravis, the thymus, a gland located in the chest, behind the breastbone, appears to be involved and plays an important role in the development of the immune system in early childhood (it produces hormones necessary for the development and maintenance of normal immune defenses) . From puberty, gland involution begins and the once functionally active thymic cells are replaced by fibrous connective tissue.
Some adult patients with myasthenia gravis have abnormal enlargement of the thymus gland or a thymoma (tumor of the thymic gland). The relationship between the thymus and myasthenia gravis is not yet fully understood, but this gland is clearly associated with the production of antibodies directed against the acetylcholine receptor.
Other considerations. The disease must be distinguished from congenital myasthenic syndrome, which may have similar symptoms but does not respond to immunosuppressive treatments.
Signs and symptoms
For further information: Myasthenia gravis symptoms
The hallmark of myasthenia gravis is the fatigue of the voluntary muscles, which worsens with repeated or sustained use. During periods of activity, the muscles become progressively weaker, while they improve after a period of rest (symptoms can be intermittent).
The muscles that control the movement of the eyes and eyelids, facial expressions, chewing and swallowing are particularly susceptible.
The onset of the disease can be sudden and, often, symptoms are intermittent. The degree of muscle weakness varies greatly between patients. Sometimes, it can present in a localized form, for example limited to the eye muscles (ocular myasthenia); in others cases, can manifest as severe and generalized symptoms, affecting many muscle groups, including those that control breathing and neck and limb movements.
Symptoms of myasthenia gravis, which vary in type and severity, can include:
- Ptosis (drooping of the eyelids): can be asymmetrical or affect both eyes;
- Double vision (diplopia): sometimes it occurs only when looking in a particular direction;
- Blurred vision: can be intermittent.
- Unsteady and swaying gait;
- Weakness in the arms, hands, fingers, legs and neck
- Chewing problems and difficulty swallowing (dysphagia), due to the involvement of the pharyngeal muscles;
- Change in facial expressions, due to the involvement of the facial muscles;
- Shortness of breath
- Dysarthria (speech impairment, often becomes nasal).
Ocular myasthenia
General symptoms
Pain is not usually a characteristic symptom of myasthenia gravis, but if neck muscles are affected, patients may experience back pain due to the effort to keep the head elevated.
Myasthenic crisis
A myasthenic crisis occurs when the upper chest muscles are involved; this represents a "medical emergency that requires hospitalization and immediate medical treatment." Severe myasthenia gravis can produce respiratory paralysis, requiring assisted ventilation. Some of the triggers for myasthenic crisis include physical or emotional stress, pregnancy, infections, fever, and adverse drug reactions.
How the disease progresses
The course of myasthenia gravis is highly variable over time and can potentially affect all the muscles of the body. However, in many cases, the disease does NOT progress to its terminal stage. For example, some patients only experience eye problems. of the disease, periods of accentuation of symptoms alternate with remissions. Myasthenia gravis may occasionally resolve spontaneously, but in most cases it is a lifelong condition. With modern treatments, however, symptoms can be well controlled.
Associated conditions
Myasthenia gravis is associated with several diseases, including:
- Thyroid disorders, including Hashimoto's thyroiditis and Graves' disease
- Type 1 diabetes mellitus;
- Rheumatoid arthritis;
- Systemic lupus erythematosus;
- Central nervous system demyelinating diseases (e.g. multiple sclerosis).
Diagnosis
Diagnosis of myasthenia gravis can be complex, as symptoms can be difficult to distinguish from other neurological disorders. A thorough physical examination may reveal easy fatigue, with weakness improving after rest and worsening on repetition of the stress test.
Myasthenia gravis is diagnosed using a number of tests, including:
- Blood test. Blood tests help identify specific antibodies (Ab), including:
- Abanti-receptor of acetylcholine;
- Ab against the muscle-specific receptor kinase (MuSK is a muscle-specific tyrosine kinase, present in some patients without antibodies to AChR);
- Ab directed against calcium channels (to rule out Lambert Eaton's myastheniform syndrome).
In most people with the disease, identification of these specific autoantibodies is sufficient to confirm the diagnosis. However, further investigation may be required.
- Electromyography (EMG). The doctor inserts a very fine needle into a muscle to measure the electrical response to nerve stimulation. In the case of myasthenia gravis, the response to repeated stimulation is atypical.
- Edrophonium Test. Injection of edrophonium chloride (Tensilon) blocks the enzyme that breaks down acetylcholine at the neuromuscular junction. In patients with myasthenia gravis, the drug can cause a sudden and temporary improvement in symptoms.
- Diagnostic for images. A chest X-ray is commonly done to rule out other conditions, such as Lambert-Eaton syndrome, often associated with small cell lung cancer. Computed tomography and magnetic resonance imaging are the best ways to identify a thymoma (thymus tumor).
Treatment
There is no specific cure for myasthenia gravis, but a number of treatments can help manage symptoms effectively.
Some of the treatment options include:
- Lifestyle changes: adequate rest and minimization of physical exertion.
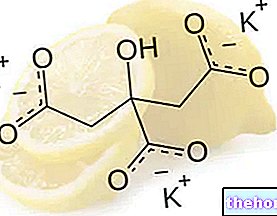
- Cholinesterase inhibitors: the treatment of choice for myasthenia gravis is the administration of a cholinesterase inhibitor (enzyme that degrades acetylcholine). Pyridostigmine, in particular, intervenes by increasing the ability of acetylcholine to compete with autoantibodies for receptors present in the end motor plates of neuromuscular junctions. The drug can temporarily improve muscle strength. The effect usually wears off within 3-4 hours, so you will need to take the tablets at regular intervals throughout the day. Possible side effects of treatment include allergies, drug interactions and overdose symptoms such as diarrhea, nausea and vomiting. Sometimes, some medication is prescribed to help reduce side effects.
- Corticosteroids: These drugs work by suppressing the activity of the immune system and reducing the production of antibodies against the acetylcholine receptor. Corticosteroids are suspected to stimulate the synthesis of a higher number of AChRs in muscle cells. Despite the good results, corticosteroids can cause more side effects than other types of therapy.
- Immunosuppressive drugs: Drugs such as azathioprine, methotrexate and cyclosporine inhibit the production of autoantibodies. This helps reduce the symptoms of myasthenia gravis. Immunosuppressive drugs can cause several side effects.
- Plasma exchange - the procedure reduces the amount of autoantibodies circulating in the body. During plasmapheresis, the plasma is separated from the blood and cleared of the Abanti-acetylcholine receptors. The blood is then re-infused to the patient. Symptoms should improve in two days, but the effects last only a few weeks (the immune system continues creating autoantibodies.) Therefore, plasmapheresis is often used for situations where symptoms need to be controlled quickly, such as to help resolve a myasthenic crisis, and are not adequate for long-term treatment.
- Intravenous immunoglobulins: A short-term management strategy involving intravenous administration of immunoglobulins (purified antibodies obtained from the plasma of blood donors). This treatment is very expensive, but it can be useful during a myasthenic crisis that impairs the ability to breathe or swallow.
- Surgical approach (thymectomy): Following surgical removal of the thymus, the patient may report some improvement in symptoms. It is unclear how thymectomy induces remission of myasthenia gravis, but research shows that the level of anti-acetylcholine receptor antibodies is reduced after surgery. However, surgical removal of the thymus is not a suitable procedure for all patients.
For further information: Drugs for the treatment of myasthenia gravis "
Prognosis
The prognosis of myasthenia gravis is greatly improved with the introduction of immunosuppressive therapy. The availability of these and other treatments has greatly reduced mortality, allowing patients to live in near-normal conditions. However, people with myasthenia gravis often have to follow the procedure. treatment regimen for an indefinite period, as symptoms generally tend to recur upon discontinuation of treatment.