Generality
Chronic gastritis is a slow and progressive inflammatory process affecting the internal wall of the stomach (or internal gastric mucosa).

The main factors favoring chronic gastritis are infections with Helicobacter Pylori.
For an accurate diagnosis, several tests are needed, including: a physical examination, a history, a stool test, a "blood test, and an" endoscopy.
Treatment includes causal therapy, drug therapy aimed at reducing / limiting stomach acid and, finally, the adoption of a dietary plan. ad hoc.
What is chronic gastritis?
Chronic gastritis is an inflammatory process affecting the internal wall of the stomach, which begins slowly over time.
It contrasts with acute gastritis, which is instead the inflammation of the stomach wall with a rapid and sudden appearance.
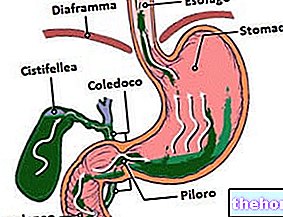
THE INTERNAL WALL OF THE STOMACH
Oriented towards the gastric lumen, the internal wall of the stomach, or internal gastric mucosa, can be divided into three layers: epithelium, lamina propria and muscolaris mucosae.
- The epithelium is the most superficial layer and has the task of secreting mucus and bicarbonate (mucus and bicarbonate have a protective function).
- The lamina propria is the intermediate layer and hosts a "wide network of glands, responsible for the secretion of acidic digestive juices necessary for the digestion process of food.
If there were no mucus and bicarbonate secreted by the surface epithelium, these acid digestive juices would cause serious damage to the internal wall of the stomach, as their level of acidity is very high. - Finally, the muscolaris mucosae, also called lamina muscolaris mucosae, is the innermost layer (therefore "more distant" from the lumen "), formed by muscle-type cells with the important task of ensuring a certain degree of movement (peristalsis) for the entire gastric mucosa.
Readers interested in learning more about the anatomy and physiology of the gastric mucosa can consult the article here.
Causes
The weakening of the mucus and bicarbonate layer and the simultaneous erosive activity of acid digestive juices, products for the digestion of food, cause the onset of chronic gastritis.
In essence, therefore, the causes of chronic gastritis are to be found in all those processes that compromise the production of mucus and bicarbonate by the surface epithelium; with the impairment of mucus and bicarbonate production, acid digestive juices are free to damage the inner wall of the stomach and cause it to erode.
FAVORING FACTORS OR RISK FACTORS
The typical conditions favoring chronic gastritis are:
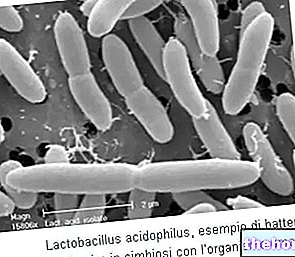
- Infections sustained by the bacterium Helicobacter Pylori. This bacterial agent lives inside the stomach (it tolerates the acidic climate present very well) and, generally, does not cause any kind of disturbance.
It can become dangerous for the health of the human being, when the immune defenses of the host organism lose their effectiveness and leave free space for bacterial colonization.
Infection with Helicobacter Pylori it is most likely the main risk factor for chronic gastritis and one of the most important conditions favoring peptic ulcer, a serious and circumscribed lesion of the mucous membrane of the digestive system.
To elevate the risk of an "infection with Helicobacter Pylori there may be a certain family predisposition to the aforementioned problem, cigarette smoking and severe stress. - Prolonged use of certain drugs, including aspirin and NSAIDs (ibuprofen, naproxen, etc.). As a result of their misuse, these medicines affect the production of mucus and bicarbonate.
- Prolonged alcohol abuse. Alcoholic substances irritate the surface epithelium, consequently also the production of mucus and bicarbonate is impaired.
- A diet that has the undesirable effect of elevating the acidity of the stomach.
Such a diet generally consists in the large excessive consumption of: fats, oils that have been cooked, citrus fruits and coffee. - Kidney failure.
- Some viral infections, such as AIDS, and some parasitic infections (parasites).
- The intense stress that some particular situations in life can cause.
For example, very stressful events for the human being, capable of inducing ailments such as chronic gastritis, are major surgery operations, serious injuries, long-term illnesses, etc. - Bile reflux. Bile reflux is the return of bile from the duodenum to the stomach and, in severe cases, to the stomach as well.
- Older age. As a result of the aging process, the surface epithelium of the inner wall of the stomach tends to deteriorate and produce less and less mucus and bicarbonate.
- Autoimmune diseases affecting the gastrointestinal tract (e.g. Crohn's disease). Autoimmune diseases are morbid conditions characterized by an exaggerated and improper response of the immune system.
For unclear reasons, in individuals with an autoimmune disease, the elements that make up the immune system (mostly cells and glycoproteins) attack perfectly healthy tissues and organs, causing even very serious damage.
Symptoms and Complications
For further information: Gastritis Symptoms
Chronic gastritis is a condition that, in some individuals, is symptomatic, while in other individuals it is devoid of evident clinical manifestations (chronic asymptomatic gastritis).
Typical symptoms of symptomatic chronic gastritis are upper stomach pain, fullness, nausea, vomiting, belching, lack of appetite, weight loss, and indigestion (or indigestion).
COMPLICATIONS OF CHRONIC GASTRITIS
In severe cases, chronic gastritis can cause: episodes of gastrointestinal bleeding, black stools and persistent stomach pain.
Main symptoms of gastrointestinal bleeding:
- Vomiting with blood (hematemesis)
- Bleeding from the rectum
- Blood in the stool
WHEN TO SEE THE DOCTOR?
An individual should contact their treating physician, when suffering from the above symptoms for more than a week.
In case of complications, it is advisable to go immediately to the nearest medical-hospital center and undergo all the necessary treatments.
Diagnosis
In general, the diagnostic process for identifying chronic gastritis and the causes that induced it begins with a careful physical examination and a careful medical history. Then, it continues with a test for the "Helicobacter Pylori(the most common contributing factor), blood tests and a stool test. Finally, it ends with an "endoscopy.
Under certain circumstances, doctors may also order a barium sulfate contrast X-ray of the digestive system.
An accurate diagnosis of chronic gastritis and of the contributing factors allows to plan an adequate and effective therapy.
OBJECTIVE EXAMINATION AND HISTORY
The physical examination is the set of diagnostic maneuvers, carried out by the doctor, to verify the presence or absence, in the patient, of the signs indicative of an abnormal condition.
The anamnesis is the collection and critical study of the symptoms and facts of medical interest, reported by the patient or his family.
Physical examination and medical history are the first step in a correct diagnosis of chronic gastritis.
HELICOBACTER PYLORI TEST
There are three different ways to detect the presence of Helicobacter Pylori: through a blood test, through a stool test and through the so-called breath test (or breath test).
Readers interested in learning more about the diagnostic methods of the "Helicobacter Pylori can consult the article here.
ENDOSCOPY
It involves the use of a tubular-shaped instrument, equipped with a camera at one end and designed for its introduction into the mouth.
The camera is connected to an external monitor, on which it projects what it sees inside the human body.
Endoscopy is extremely useful for at least two reasons:
- Look for any signs of inflammation
- It allows the collection of pieces of tissue, from the inner wall of the stomach, in order to perform a biopsy. To pick up pieces of fabric, the instrument must be equipped with a special collector element (a sort of small chisel).
Treatment
Generally, the treatment of chronic gastritis includes a therapy focused on treating the causes / favoring factors (causal therapy), a drug therapy aimed at reducing / limiting the acidity of the stomach and, finally, the adoption of a dietary plan that does not cause an "excessive production of acidic digestive juices by the gastric mucosa.
CAUSAL THERAPY
Causal therapy varies based on what the treating physician has identified as a trigger or factors for chronic gastritis.
For example, if from the various diagnostic tests it emerged that at the origin of the symptoms there is an infection with Helicobacter Pylori, the causal therapy would consist of a treatment based on antibiotics.
PHARMACOLOGICAL THERAPY
Typical drugs for chronic gastritis (regardless of the favoring factors found during diagnosis) consist of:
- Antacids. They are useful for buffering gastric acidity (ie stomach acidity) and relieving disorders related to poor digestion (eg heartburn).
Often, doctors associate their administration with an administration of H2 blockers or proton pump inhibitors.
Classic examples of antacids indicated in case of chronic gastritis are magnesium hydrate and aluminum hydroxide. - Anti-H2 (or H2 receptor antagonists). They have the effect of reducing the stomach's production of acidic digestive juices.
A typical H2 blocker used in chronic gastritis is ranitidine. - Proton pump inhibitors (PPIs). They act in a very similar way to H2 receptor antagonists, so they reduce the production of acid secretions in the stomach.
Typical PPIs administered in chronic gastritis are pantoprazole and lansoprazole.
DIET: MAIN ADVICE
The foods to avoid in the presence of chronic gastritis are fried foods (which contain a high percentage of fat), fatty foods, citrus juices, coffee and alcohol, while the recommended foods are: all vegetables, fruit (with the exception of citrus fruits, of course), low-fat food products, lean meats (e.g. chicken or turkey meat), pasta and rice (NB: pasta and rice prepared, of course, in "light" way).
Diet control can have unexpected beneficial effects, which is why doctors recommend that you always pay close attention to it.
Prognosis
The prognosis in chronic gastritis depends on the curability of the contributing factor (s) and on how early the treatments started.
In fact, a chronic gastritis, whose favoring conditions are easily treatable, has a better prognosis than a chronic gastritis characterized by hardly treatable favoring conditions or a form of chronic gastritis that is treated late.
RELAPSES: WHO IS MOST AT RISK?
Chronic gastritis is a condition that, even if treated properly, can recur after some time.
The risk of relapse (or relapse) is greater in patients who, after recovery, tend to pay less attention to the diet and restart with the intake of "prohibited" or "not recommended" foods during the treatment phase.
Prevention
Avoiding the intake of foods that stimulate the production of acidic digestive juices, limiting the consumption of alcohol, taking NSAIDs and aspirin only when strictly necessary and learning to control stress are the main preventive measures, which doctors recommend to reduce the risk of chronic gastritis.













.jpg)