Caused by factors not yet fully understood, intestinal endometriosis manifests itself, in symptomatic cases, with: abdominal pain during defecation and bowel movements, recurrent pelvic-abdominal pain, abdominal cramps, diarrhea alternating with constipation, etc.
The diagnosis of intestinal endometriosis is not simple and requires several investigations.
Therapy varies according to factors such as the severity of the symptoms and the willingness or not of the patient to seek pregnancy in the future.
Typical of women of childbearing age, endometriosis is one of the most common causes of chronic pelvic pain.
Despite numerous studies on this subject, endometriosis continues to remain a largely unknown condition, especially as regards the causes and its consequences on fertility.
Ectopic Endometrium
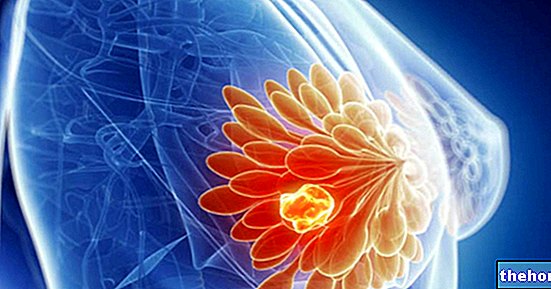
The ectopic endometrium is the endometrium which, in endometriosis, grows outside the uterus and in inappropriate parts of it.
The ectopic endometrium behaves exactly like the physiological endometrium that covers the inner wall of the uterus; this means that, about once a month, in women still menstruating, it disintegrates under the influence of the hormones of the menstrual cycle, giving life to bloody and painful lesions.
The endometrium
Highly vascularized and rich in muciparous glands, the endometrium represents the innermost cellular layer of the uterus as well as its mucous membrane.
Due to the effect of estrogen and progesterone - the hormones secreted by the ovaries during the menstrual cycle - the endometrium is renewed regularly, thus ensuring the constant presence of an environment suitable for the implantation of an embryo.
The implantation of these cells inside the abdominal-pelvic cavity is responsible for the phenomenon also known as "endometriotic islets".
The theory of lymphatic and blood dissemination is the most accredited hypothesis, to explain all the presence of endometrium outside the pelvic cavity and which cannot depend on retrograde transport.
The theory of genetic predisposition is based on the observation that a not negligible number of women with endometriosis have a first relative (obviously female) affected by the same condition.
N.B: the causal theories proposed are valid for any type of endometriosis.
Intestinal Endometriosis Risk Factors
Some evidence suggests that the risk of developing intestinal endometriosis (and, more generally, the phenomenon of "endometriosis) is greater in the case of:
- Nulliparity. It is the medical term used to refer to women who have never given birth;
- Menarca (ie the first menstruation) at an early age;
- Menopause at a very old age;
- Short menstrual cycles (for example, lasting less than 27 days);
- Very prolonged menstruation (lasting more than 7 days);
- High levels of estrogen in the body or an "exposure to estrogen that adds to the amount of estrogen produced normally by the body;"
- Heavy consumption of alcohol;
- Family history of endometriosis;
- The presence of any medical condition that prevents the normal passage of menstrual flow outside the body;
- The presence of uterine anomalies.
Types of Intestinal Endometriosis
Intestinal endometriosis can affect:
- The large intestine tract immediately preceding the rectum (sigmoid and / or descending colon).
- The rectum (which is always part of the large intestine); sometimes, this variant of intestinal endometriosis also affects the vagina (recto-vaginal endometriosis).
- The ileocecal appendix (belongs to the very first tract of the large intestine).
- The small intestine.
Furthermore, intestinal endometriosis can be distinguished as superficial or deep: it is superficial, when the ectopic endometrium that distinguishes it has grown on the external surface of the intestine; it is deep, however, when the ectopic endometrium has managed to penetrate the wall intestinal.
Epidemiology
According to some reliable sources, about one third of women suffering from endometriosis would have portions of the endometrium in the intestine; Add to this that, according to a 2018 statistic, the intestine would be, after the organs of the genital system (eg fallopian tubes, vagina, etc.) the most common site of endometriosis.
In most cases (about 90%), intestinal endometriosis concerns the tract of the large intestine called the rectum or the tract immediately preceding it (sigma); more rarely, it affects the appendix and / or the small intestine.
;Due to symptoms such as abdominal pain during defecation and alternating between diarrhea and constipation, intestinal endometriosis is often mistaken for a well-known and common digestive condition that causes similar problems: irritable bowel syndrome (or "irritable bowel).
Variability of Intestinal Endometriosis
Like other forms of endometriosis, intestinal endometriosis also tends to vary in symptomatic presentation from patient to patient; in practical terms, this means that every woman with intestinal endometriosis represents a case in itself.
Complications of Intestinal Endometriosis
Intestinal endometriosis can cause the formation of one or more endometriotic cysts and / or adhesions; moreover, it can impair the ability to conceive resulting in infertility.
Sterility in Endometriosis
Several studies have shown that infertility (ie the inability to conceive) is a complication of endometriosis which affects about 30-40% of patients; this means that it is quite common.
, physical examination, gynecological examination, diagnostic imaging (transvaginal or transrectal ultrasound, magnetic resonance, CT) and, sometimes, complex procedures such as sigmoidoscopy and / or laparoscopy for diagnostic purposes.
The professional figure in the medical field who has the skills to identify a condition such as intestinal endometriosis is the gynecologist.
Gynecological examination
The gynecological examination consists in a physiological and pathological evaluation of the female genital system; in particular, the doctor who performs it is responsible for observing and palpating the external (vulva, large and small lips) and internal (vagina and cervix) genitals.
Imaging diagnostics, sigmoidoscopy and laparoscopy: what are they for?
Diagnostic imaging and, when necessary, sigmoidoscopy and laparoscopy serve not only to ascertain the presence of intestinal ectopic endometrium, but also to establish the extent and severity of intestinal endometriosis.
How to recognize asymptomatic intestinal endometriosis?
When intestinal endometriosis is asymptomatic, its detection often occurs purely by chance, during abdominal examinations or surgery performed for other reasons.
and / orImportant!
Conservative therapy for intestinal endometriosis does not eliminate the ectopic endometrium in any way; in fact, it only allows you to control the symptoms.
Pain Relief Drugs
Among the most prescribed pain relievers in case of intestinal endometriosis, paracetamol and ibuprofen, an NSAID, are reported.
Like all medicines, inappropriate use of the above medicines can have side effects, sometimes even very serious ones; therefore, it is best to consult your doctor before taking them.
Hormonal therapy with anti-estrogenic action
Hormonal therapy with anti-estrogenic action aims to control estrogen levels, in order to reduce the extent of the flaking of which the intestinal ectopic endometrium is subject to each menstrual cycle.
The drugs used for hormonal therapy with anti-estrogenic action include:
- The derivatives of progesterone, also known as progestins (eg: norethindrone and medroxyprogesterone);
- The derivatives of androgens (eg: danazol and gestrinone);
- Luteinizing hormone release stimulating hormone synthetic analogues, also known as LH-RH synthetic analogues (eg: leuprorelin, goserelin, triptorelin and leuprolide).
Surgical Treatment of Intestinal Endometriosis
The surgical treatment of intestinal endometriosis aims to eliminate, as far as possible, the ectopic endometrium; it is indicated when conservative therapy is ineffective or in case of female sterility due, most likely, to the ectopic endometrium.
Currently, three different types of surgery are available for the elimination of the ectopic endometrium from the intestine:
- Segmental bowel resection surgery.It involves the removal of the segment of intestine affected by the ectopic endometrium, followed by the rejoining of the two remaining organ stumps.
- The "shaving" procedure. It consists in shaving the ectopic endometrium portion, without involving the intestine in any way; its execution inevitably leaves some traces of unwanted endometrial tissue.
- Discoid resection surgery. It is used when the ectopic endometrium is small in size and involves the removal of the intestine area on which the aforementioned endometrial tissue resides, followed by the closure of the resulting hole.
The choice of the type of surgery to be adopted is up to the treating gynecologist, who decides on the basis of the extent and severity of the intestinal endometriosis.
There are two possible techniques for performing surgical interventions for intestinal endometriosis: laparoscopy (which is minimally invasive) and laparotomy (which instead involves an "important abdominal incision).
After surgery for intestinal endometriosis, there is a period of hospitalization of a few days, during which the medical staff constantly monitors the patient's condition; once home, it may take several weeks for complete recovery.