Generally, knee osteoarthritis is the result of a combination of circumstances; rarely, it depends on only one cause. Among the factors that favor the development of knee osteoarthritis, stand out: old age, obesity, a history past of knee injuries and meniscus removal operations.
More often bilateral than unilateral, knee osteoarthritis typically causes: knee pain, joint stiffness, redness of the skin at the knee, creaking from the knee, swelling, and reduced joint mobility.
Unfortunately, at the present time, knee osteoarthritis is a condition with irreversible effects and for which there are only symptomatic treatments.
Brief anatomical recall of the Knee
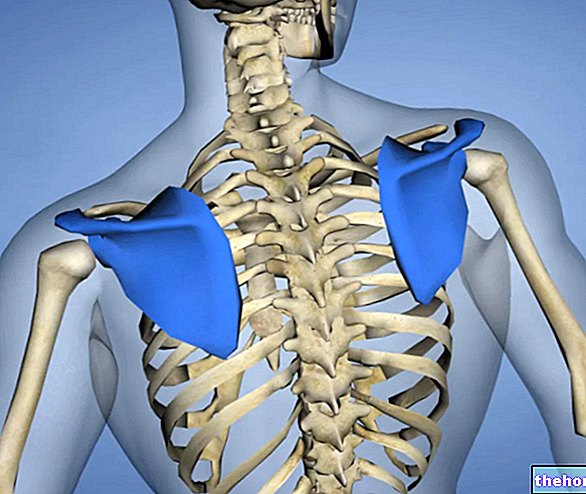
The knee is the important synovial joint of the human body, located between the femur (superiorly), tibia (inferiorly) and patella (anteriorly).
Its anatomy is quite complex and includes:
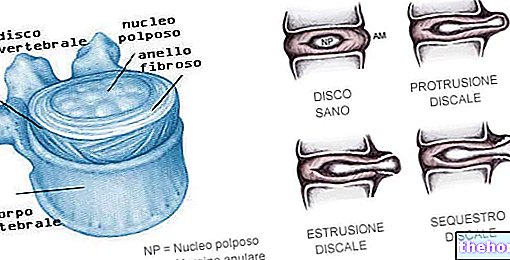
- The articular cartilage, which covers the lower surface of the femur, the inner side of the patella and the center of the upper surface of the tibia, protecting all these bones from mutual friction;

- The synovial membrane, which covers the joint from the inside and produces the synovial fluid, a fluid with a lubricating action for all the internal structures of the knee;
- Tendons and ligaments, which guarantee joint stability and correct alignment between the femur and tibia;
- The synovial bags, which are small sacs of synovial membrane, filled with a lubricating fluid very similar to synovial fluid;
- The internal meniscus (or medial meniscus) and the external meniscus (or lateral meniscus), which are pads of cartilage with a cushioning and anti-friction function, located on the upper surface of the tibia.
In the medical field, osteoarthritis of the knee is the condition also known as gonarthrosis or osteoarthritis of the knee.
Did you know that ...
With its position and its structural components, the knee plays a fundamental role in supporting the weight of the body and in allowing the movements of extension and flexion of the leg, during a walk, a run, a jump, etc.
Arthrosis or Osteoarthritis: what is it?
In medicine, the term arthritis refers to any condition of an inflammatory nature affecting one or more joints (usually joints of the synovial type).
Osteoarthritis is a form of arthritis; to be precise, it is a form of "wear and tear" arthritis of the articular cartilages.
Of the numerous forms of existing arthritis, osteoarthritis is the most common: in the United States alone it affects 27 million people!
The normal aging process produces the generalized degeneration of the cartilages of the human body and reduces the body's ability to counteract this degeneration;
Among the sports most at risk of knee osteoarthritis, the following stand out: football, rugby, basketball, running on rough roads, skiing, American football, volleyball and tennis:
Pathophysiology: How does Knee Arthrosis originate?
In "knee osteoarthritis," inflammation results from degeneration and consequent thinning of the knee cartilages. In fact, with the degeneration and thinning of the aforementioned cartilages, the lower surface of the femur and the upper surface of the tibia collide and, thanks to the continuous rubbing due to the movements of the lower limb, they cause each other the damage from which the inflammatory condition in question.
In essence, therefore, in gonarthrosis, inflammation is the result of repeated and damaging rubbing of the femur on the tibia, after the protective cartilage layer has thinned on the lower surface of the first and the upper surface of the second.
- Knee pain. It is the predominant symptom of knee osteoarthritis; it consists of a sensation that increases with excess movement and physical activity, and that subsides with rest.
Normally, very intense pain is indicative of very severe inflammation and significant degeneration of the articular cartilage;

- Joint stiffness and reduced joint mobility. They are mainly present in the morning, just after waking up, and after long periods of immobility (eg after a car trip lasting several hours).
The stiffness of the knee and the reduction of its mobility make activities such as climbing stairs, getting up from a chair, getting in and out of the car, etc. difficult. - Redness and warmth at the knee.
- Swelling in the knee
- Emission of sounds from the knee, such as creaks or crackles, with every movement of the lower limb;
- Formation of osteophytes inside the knee. Similar to a rose thorn, beak or claw, osteophytes are small bony growths that develop on the articular surfaces of bones subjected to chronic erosive and irritative processes.
In slang, osteophytes are also known as bone spurs; - Unstable knee
- Atrophy of the thigh muscles (i.e. decreased muscle tone in the thigh). This happens because, due to pain, stiffness and the reduction of joint mobility, the patient tends more and more to a sedentary lifestyle.
Did you know that ...
According to some experts in knee osteoarthritis, humid weather and low pressure would cause knee pain and joint stiffness to worsen.
This phenomenon would be attributable to a marked sensitivity on the part of the nerve fibers that reach the joint capsule towards changes in atmospheric pressure and humidity.
Knee Osteoarthritis: Mono- or Bilateral?
Knee osteoarthritis can affect one (unilateral knee osteoarthritis) or both knees (bilateral knee osteoarthritis). However, it should be noted that, in more than half of clinical cases, it is bilateral.
Complications
In its most advanced stages, knee osteoarthritis can cause deformation of the lower limbs (knee varus).
Furthermore, when the associated symptomatology is very severe, it is an obstacle to the most banal daily activities, which often induces a state of depression and discomfort in the patient.
When to see a doctor?
An individual with suspected knee osteoarthritis should contact their doctor or an orthopedic expert in knee diseases, when joint pain and stiffness are such as to prevent the simplest daily activities from being carried out (e.g. climbing stairs, getting into a car etc.).
; then, it continues with an evaluation of the family history, to understand if there is a recurrence of gonarthrosis in the patient's family; finally, it ends with X-rays and nuclear magnetic resonance imaging (MRI) of the knees.
X-rays: what are they for?
In the diagnosis of knee osteoarthritis, X-rays serve to clarify whether the aforementioned inflammatory condition is associated with osteophytosis. In the medical field, the term osteophytosis indicates the process of formation of the aforementioned osteophytes at the joint level.
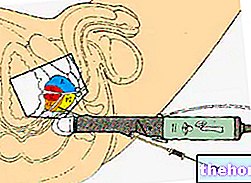
Magnetic Resonance: what is it for?
Among the various investigations necessary for the diagnosis of gonarthrosis, the nuclear magnetic resonance of the knee is, in all probability, the most significant and reliable. In fact, it not only ascertains what emerged in the previous diagnostic tests, but also allows us to clarify the extent of the degeneration and thinning of the cartilages of the femur and tibia.
The information deriving from the nuclear magnetic resonance imaging of the knees allows the attending physician to determine the most appropriate treatment.
Symptomatic Therapy for Knee Osteoarthritis: what does it consist of?
Symptomatic therapy for knee osteoarthritis can be conservative (or non-surgical) or surgical.
Generally, doctors give priority to symptomatic treatments of a conservative nature, reserving the right to resort to surgery only if the conservative practice has not provided any results (or the results provided are unsatisfactory and the patient continues to experience intense pain, joint stiffness, swelling, etc.) .
CONSERVATIVE SYMPTOMATIC THERAPY
Conservative symptomatic treatments for knee osteoarthritis include:
- A diet plan aimed at reducing body weight. This obviously applies when an overweight / obesity condition has contributed to the onset of gonarthrosis;
- Physiotherapy exercises aimed at strengthening the muscles of the lower limbs (thigh in particular) and increasing the joint mobility of the knee.
A stronger thigh musculature relieves the load of body weight on the knee, with enormous benefits for the latter.

- The administration of pain relievers and non-steroidal anti-inflammatory drugs (i.e. NSAIDs). Among the painkillers and NSAIDs most used in the case of osteoarthritis of the knee, paracetamol, ibuprofen and naproxen sodium are reported.
The use of these medicines is beneficial in a good number of patients. - Injections into the knee of corticosteroids and / or hyaluronic acid. Corticosteroids are powerful anti-inflammatories, whose prolonged or inappropriate use can give rise to serious side effects (hypertension, obesity, glaucoma, etc.); for this reason, doctors prescribe them only in case of real need and only when NSAIDs are ineffective.
Hyaluronic acid, on the other hand, is a lubricating substance, physiologically present inside the synovial joints such as the knee; with its administration, doctors intend to restore part of the normal joint structure, which has disappeared due to arthrosis. - The practice of moderate but constant physical exercise for the lower limbs. The purposes of this physical exercise are, in fact, the same as those of physiotherapy.
Contrary to what one might think, immobility and sedentary lifestyle are only apparently a source of benefits for the patient with osteoarthritis of the knee.
Clearly, physical exercise must be targeted and must not, in any way, cause further damage to the knees. - The use of a specific brace for the diseased knee. There are various types of braces for the knee affected by arthrosis; the choice of the most suitable brace is up to the treating orthopedist and generally depends on the state of health of the joint interested.
SURGICAL SYMPTOMATIC THERAPY
There are at least three different surgical approaches to address knee osteoarthritis; these approaches are:
- The "cleaning" of the cartilage of the knee carried out in arthroscopy. It is the least invasive option, but also the least effective. Generally, orthopedists reserve it for younger patients with early knee osteoarthritis.
- Osteotomy of the femur or tibia. Osteotomy is a surgical procedure that involves the remodeling of a particularly deteriorated joint bone, in order to better redistribute body weight inside the joint.
Generally, knee osteotomy is reserved for patients with damage to the cartilage of only one of the two bony portions forming the joint. - The installation of a prosthesis in place of the real knee. The installation of a knee prosthesis is a very invasive and delicate surgery; however, if successful, the benefits for the patient are more than appreciable.
Although the most modern knee prostheses now last up to 20 years, still today orthopedists only recommend them to elderly patients (aged 55 and over).