In man, the synthesis of testosterone occurs in large part (95% ca) at the level of the testes, in particular in the interstitial cells of Leydig. These cells are arranged in isolation or in small groups in the stroma that surrounds the contorted seminiferous tubules, responsible for spermatogenesis Together, the Leydig cells represent the so-called interstitial gland, the seat of production of androgenic steroid hormones, including testosterone.
Polyhedral and often irregular in shape, the interstitial cells of Leydig synthesize testicular steroids starting from cholesterol carried by LDL or synthesized in the cell starting from acetate (through Beta-oxidation). During the steroidogenesis process, which takes place at the mitochondrial level. , cholesterol is converted to pregnenolone and subsequently to DHEA, Androstenedione and testosterone.
- The main testicular steroid produced by Leydig cells is testosterone, then we have androstenedione, DHEA, DHT and estradiol (E2).
95% of testosterone is produced in the testicles, while DHT and estradiol derive for 80% from the peripheral conversion of precursors of testicular and adrenal origin, and 20% are produced in the testis.
The synthesis of testicular steroids (steroidogenesis) occurs following stimulation by the LH of the receptors expressed by the Leydig cells (for this reason, in the male LH is also called Interstitial Cells Stimulating Hormone, ICSH).
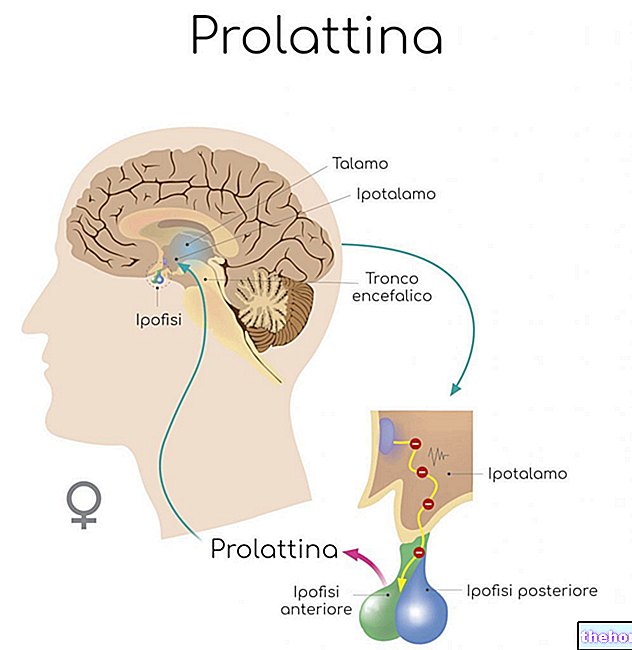
Being the secretion of LH by the pituitary in response to the hypothalamic GnRH (Gonadotrophin Releasing Hormon) of the pulsatile type, testosterone production in the testis is also discontinuous. However, it should be noted that the response of the testis to the LH stimulus is late (24-72 h).
The production of testosterone in the testes is strictly dependent on the hypothalamus and the pituitary; we therefore speak of the hypothalamus-pituitary-testicle axis.
- the GnRH secreted by the hypothalamus reaches the gonadotropic cells of the adenohypophysis where it binds to specific membrane receptors, stimulating the secretion of LH and a small part of FSH, which occurs in a pulsatile manner:
- at the level of the testes, LH determines the synthesis of testosterone by the Leydig cells favoring the conversion of cholesterol into pregnenolone up to the production of testosterone → testosterone directly inhibits the synthesis and hypothalamic release of GnRH and pituitary LH (feed control) back).
- FSH binds to specific membrane receptors located on the surface of Sertoli cells, stimulating the release of various proteins and hormones → these substances (inhibin) suppress on the one hand the hypothalamic release of FSH and on the other support the maturation of spermatozoa . FSH also acts on the germline cells contained in the seminiferous tubules, stimulating the maturation of spermatozoa, which also requires adequate concentrations of testosterone.
- The small amount of estradiol produced at the testicular level and that deriving from the peripheral conversion of androgens (aromatase) acts at the hypothalamic and pituitary level, reducing the amplitude of the spontaneous pulsations of LH.
- Prolactin stimulates the production of androgens by Leydig cells and enhances their action by increasing the sensitivity of the target tissues; however, in the case of hyperprolactinemia, opposite effects occur.
From the above it is clear that the endocrine activity of the Leydig cells is supported by the supporting or Sertoli cells, located in the wall of the seminiferous tubules alongside the germ cells used for spermatogenesis, that is, for the synthesis of male spermatozoa or gametes.
The Sertoli cells perform numerous functions, including maintaining the architecture of the seminiferous tubules and guaranteeing metabolic exchanges with the germ cells for the coordination of spermatogenesis; all this thanks above all to the endocrine activity with which the Sertoli cells produce:
- ABP: a protein that binds testosterone and DHT, increasing their concentration at the tubular and epididymal level; therefore it favors spermatogenesis.
- inhibin: acts at the pituitary level where it selectively inhibits the secretion of FSH
- estrogens: deriving from the aromatase metabolization of testosterone produced by the nearby interstitial cells of Leydig