"Liver biopsy
Is the exam painful?
Although it literally runs out in a second or so, given the preparatory phase, the liver biopsy takes an average of 15-20 minutes.
During the collection, the patient may feel a slight pain or a sensation of pressure on the skin.
In any case, thanks to the preventive local anesthesia, the examination is generally well tolerated.
After a liver biopsy

At the physician's discretion, the subject will then be discharged in the evening or the following day.
During the stay in the outpatient clinic (day hospital) the patient may complain of slight pain in the place where the puncture was performed, sometimes radiating to the shoulder.
Their onset, linked to a slight irritation of the pleura and peritoneum (membranes that envelop respectively the lungs and most of the viscera), can be easily controlled by administering pain-relieving drugs. Furthermore, once the liver biopsy is completed, a further phase of fasting lasting at least six hours is foreseen.
As a rule, antibiotic coverage is not necessary, while the patient is subjected to constant monitoring of heart rate and blood pressure, to detect early the eventual and rare eventuality of hepatic haemorrhage.
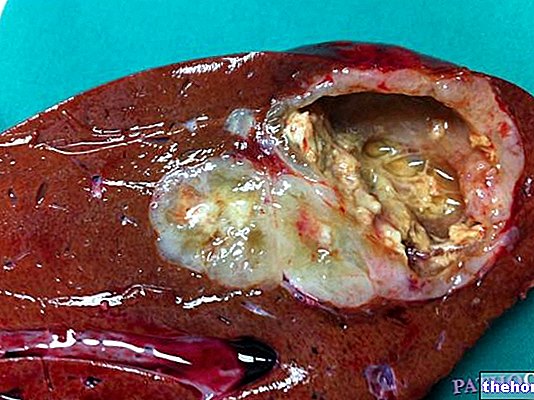
The liver fragment taken by the hepatologist is sent to the laboratory for examination under the microscope by another specialist, the pathologist. As a rule, the result of the biopsy is available after one or two weeks.
After discharge, it is preferable to be accompanied home by a family member, avoiding driving. This advice becomes mandatory in the event that the doctor has administered sedative drugs, and in this case it applies for about 12 hours from the end of the procedure.
Back home, the patient must absolutely avoid physical exertion for the first 24 hours. The next night will be spent in absolute rest and - as a precaution - preferably near a hospital (no more than 30 minutes away). In the presence of pain, the patient will have to agree in advance with the doctor how to take the most suitable drugs; for example, all painkillers that interfere with the blood clotting process are contraindicated.
Risks and Complications
Despite being an invasive and bloody examination, liver biopsy is a procedure with a high margin of safety, which does not involve risks for the patient. Serious complications are in fact quite rare. The most common, certainly not serious because it is easily manageable, is post-surgery pain, which affects up to 20-25% of patients, localizing on the puncture site (the upper right part of the abdomen) and spreading quite often to the right shoulder. . Another frequent complication, which should not cause too much concern, is the drop in blood pressure (10% of patients). The lowering of pressure is usually due to a reaction called vaso-vagal, during which the blood vessels dilate and the heart your frequency decreases. This episode is very similar to what happens during a fainting, so the patient may complain of blurred vision, weakness and a sense of fainting.
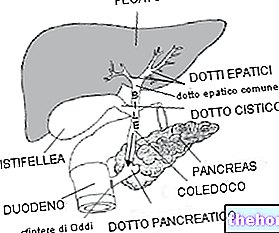
Among the most serious complications, which may require surgery and transfusion therapy, we remember bleeding (one case in 500-1000 biopsies), which can be mild or more rarely (one case in 2000) severe, to the point of requiring hospitalization. with embolization procedures and possible transfusion. The mortality risk associated with liver biopsy is very close to zero (one case in 10,000-12000). A further, possible complication is the accidental puncture of a nearby bowel (one case in 3000), while theoretically there is also a potential risk of spreading tumor cells or spreading infectious processes. Transjugular liver biopsy is associated with a further risk represented by adverse reactions to the contrast medium; it also involves the use of X-rays, so it is not recommended for women of childbearing age.
Preparation for surgery
The liver biopsy is performed fasting, for which the patient is explicitly requested not to eat and drink in the six hours preceding the examination. The subject must present himself with pajamas, slippers and all the documentation relating to the previous checks.
Sufficiently in advance, the patient will have to inform the doctor about the medicines usually taken, as well as about any allergies or illnesses in progress. The therapy with anticoagulants or drugs that interact with sedatives can in fact be temporarily suspended in view of the examination (usually for a week). for high blood pressure, antibiotics, anti-asthmatics, NSAIDs (such as aspirin, ibuprofen and naproxen) and also some food supplements (garlic, ginkgo biloba and fish oil).
Before the liver biopsy, the patient may undergo a small blood sample to determine his coagulation capacity, often poor in subjects with severe liver dysfunction. To avoid bleeding episodes, if necessary, concentrates of coagulation factors can therefore be administered.
Once all the information relating to the techniques used and the risks they entail has been received, the subject must sign the so-called informed consent.
Since the patient will not get out of bed for about 4 hours after the liver biopsy is finished, it is wise to go to the toilet before it begins.