«Diet As a Cause of Hepatitis
After having illustrated the role of nutrition as a possible cause of various types of hepatitis, we try to understand what are the objectives of a diet aimed at treating liver disease.

Strange as it may seem, in many cases it is NOT possible to pursue all the above objectives at the same time; a choice between the various possibilities is therefore necessary. This decision (ALWAYS and ONLY at the DISCRETION of the TREATMENT SPECIALIST DOCTOR) must be made according to some primary factors, which are: severity of the hepatitis, functionality and insufficiency of the organ, other comorbidities, prognosis and subjective characteristics of the patient, etc. Definitively, there is NO ONE diet for hepatitis, since this must be established according to the situation; it is therefore no coincidence that various diets for hepatitis can also be almost diametrically opposed to each other. Furthermore, although they are potentially (but not necessarily!) Related, it is necessary to specify that "hepatitis" and: LIVER INSUFFICIENCY, HEPATIC FIBROSIS, HEPATIC CIRRHOSIS or LIVER CARCINOMA are NOT synonymous! It is in fact possible that severe acute hepatitis causes transient but treatable liver failure, or that chronic hepatitis does not induce liver failure but tends to slowly evolve into fibrosis and then into cirrhosis. to a mild but stable cirrhotic state.In short, the possibilities are really many!
In any case, among all this necessary variability, there are some UNIVOCALLY shareable rules, which are:
- ABOLITION of ALCOHOL
- ABOLITION of DRUGS and food SUPPLEMENTS NOT NECESSARY
- ABOLITION / REDUCTION to the minimum terms of OTHER NERVINS (coffee, tea, chocolate ...) and of SALT (and, if desired, also of SUGAR) ADDED
- ABOLITION of Junk or FAT FOOD or in any case rich in REFINED SUGARS
- REGULARIZATION of meals and TREND to NUTRITIONAL BALANCE (both FASTING and EXCESS CALORIES FORBIDDEN, especially if over 10% of the calorie level).
ATTENTION! The article refers to the DIET understood as nutrition FOOD for hepatitis, therefore, it excludes ENTERAL and PARENTERAL nutrition! Obviously, in case of severe hepatitis (or in any case in the midst of acute symptoms), the use of parenteral is more usual; however, in the long periods of artificial feeding, the use of enteral feeding is increasingly indicated, which guarantees the maintenance of the functionality of the various digestive organs.
First, we will analyze the diet for alcoholic and / or food steatohepatitis; then, the diet for hepatitis will be described WITHOUT severe impairment of liver function. Finally, we will mention the basic nutritional principles for hepatic degeneration and the complications to which it is associated (ascites, encephalopathy, portal hypertension, haemorrhages, etc.).
Diet for Alcoholic and / or Alimentary SteatoHepatitis - Diet for Fatty Liver
Steatohepatitis is the most common liver disorder in the populations of industrialized countries.
The diet for this hepatitis (which can be acute or chronic depending on the case) is, to be honest, very simple. First, it is FUNDAMENTAL to remove the etiological origin of steatosis, ie alcohol abuse on the one hand and food abuse on the other (possibly both!). Then, since it is a condition frequently linked to overweight / obesity, the diet should be associated with a program of physical motor activity and acquire a certain slimming effect; ultimately, the diet for fatty steatosis is often a low-calorie diet that subtracts 30% of the total energy needed to maintain normal weight.
The nutritional organization is quite rigid, especially as regards the absence of alcohol, sweet foods and junk foods. The abolition of added sucrose (and of the foods containing it), and of cooking salt (as well as of the foods that include it) is required. The main lipid source is extra virgin olive oil, the protein one is mixed, therefore composed of animal and vegetable foods, while simple sugars are ONLY contained in vegetables in raw form and in dairy products (fruit, vegetables, semi-skimmed milk and natural yogurt). All cereals are whole and possibly whole (not in the form of flours and derivatives); however, these must be alternated with legumes, obtaining a grain-legume ratio of 2: 1 or even 1: 1. The vegetables, to be eaten in alternating raw and cooked form, are in season and in portions ranging between 100 and 200g for both lunch and dinner. Fruit and yogurt alternately structure secondary meals.
The breakdown into energy nutrients is balanced, that is: about 1g / kg of DESIRABLE PHYSIOLOGICAL weight in proteins, 25% of lipids with the greatest possible amount of unsaturated (omega3 / omega6 ratio 1: 4 - omega 9 in abundance), and the rest of energy in totally complex carbohydrates, with the exception of fructose and lactose in food. Respecting individual susceptibility, the fiber must reach 30g / day and both mineral salts and vitamins must comply with the correct recommended rations. meals must be at least 5 and with the same caloric breakdown of a balanced diet: 15% for breakfast, 5-10% for the two snacks, 35-40% for lunch and 30-35% for dinner.
In restoring hepatic integrity, all the plant molecules with phyto-therapeutic action (therefore antioxidant, cholesterol-lowering, hepatoprotective, etc.) acquire a very important role; among these: plant lecithins, phytosterols, phenolic substances, etc. In particular, phenolic substances they must be abundant, perhaps with a good content of cinarina (i.e. a polyphenol contained in artichokes) e silymarin (a phenolic complex abundantly contained in milk thistle). The intake of provitamin A, vitamin C and vitamin E also favors the improvement of the liver condition (especially C).
In the case of alcoholic steatosis, since alcoholism causes intestinal malabsorption and the reduction of vitamin stocks (if any!), The subject could significantly benefit from generic food supplementation and above all from thiamine (vitamin B1).
Diet for Hepatitis Without Serious Impairment of Liver Function
After the previous one, the diet for hepatitis without serious compromises is certainly the most used. It includes all forms of acute or chronic infectious / parasitic hepatitis. It has an enormous application in the treatment of chronic virus hepatitis. HBV (which affects about 350,000,000 people in the world) and has many aspects in common with the one already described.
Compared to the diet for food or alcoholic fatty steatohepatitis, this does not require you to "empty" the liver cells of excess fat and glycogen. It goes without saying that, albeit desirable, motor activity fades into the background or is totally abolished in acute forms and, except for the presence of other comorbidities, the same applies to slimming capacity.
On the other hand, some precautions already mentioned are much more important, such as the abolition of alcohol, unnecessary drugs and supplements, and the absolute moderation of other nerves, salt, sugar and junk foods. In addition, despite what one might believe, it is essential to AVOID fasting or excessive calorie REDUCTION, as well as overeating and excess energy.
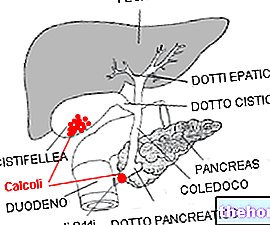
The liver is the organ responsible for many metabolic functions, including gluconeogenesis, lipogenesis and proteosynthesis; but also for the production of digestive bile. By virtue of the fact that, in the case of hepatitis, it is necessary to reduce as much as possible the "amount of work" of the organ (for blood homeostasis and digestion), the diet must necessarily be NORMALcaloric. Fasting or an insufficient diet REQUIRE a greater hepatic effort than normal, since the organ must produce glucose (essential for the central nervous system) starting from glycerol and circulating amino acids. Furthermore, we remind you that prolonged hypo-nutrition (and above all the depletion of carbohydrates) determines the accumulation of ketone bodies, potentially TOXIC molecules for all tissues. Not least, an insufficient diet DOES NOT allow the intake of essential amino acids in quantities sufficient for protein synthesis; the liver, already less efficient because it is sick, if it is not supplied with these substrates, finds it difficult to produce all the protein molecules of the plasma.On the other hand, an energy surplus involves other drawbacks: first of all, hepatocytes must increase biliary production for the emulsion of fats in digestion. Secondly, excess amino acids and carbohydrates in the diet require conversion to fatty acids by the liver; here, again, there is an increase in the total WORK of the organ (without considering the possible tendency to fatty steatosis).
It is then necessary to make a final clarification on the relevance or otherwise of other molecules in the diet. In my opinion, in the nutritional regimen for hepatitis, it is also strongly advisable to significantly limit the concentration of certain additives (especially sweeteners and preservatives). We reiterate for the umpteenth time that the liver is responsible for the metabolization of most nutritional molecules and circulating in the blood, which is why it is conceivable that the excess of these synthetic products requires a greater effort on the part of the organ.
Finally, I would like to focus on a generally unknown but far from negligible detail, namely the use of fructose as a sweetener. It must be clear that I am not talking about fructose NATURALLY present in foods (fruit and vegetables), but about the granular one. This, which is not well oxidizable by human cells, must necessarily be converted by the liver into glucose. While that naturally introduced with raw foods reaches percentages ranging from 10 to 16% of total calories, using sweetened foods, sweetening drinks and granular fructose for seasoning, this value can even double.
The breakdown of macronutrients is the same as in the previous diet, as is the energy breakdown of meals. Again good amounts of antioxidants and dietary supplementation with vitamins can be of great help.
Notes on the Nutritional Needs of Hepatic Insufficiency
Hepatic insufficiency can be mild, moderate or severe, and also present "it" (in combination with hepatitis) in an acute or chronic form. It is necessary to take into account, first of all, that hepatic insufficiency is characterized by a reduction of the functions of the organ.
In mild forms, frequently supported by traditional nutrition and not by artificial nutrition, it is advisable to use easily digestible meals, with moderate portions, but without neglecting the overall nutritional intake.
On the other hand, starting from the moderate form and ending with the severe one (often subject to enteral or parenteral nutrition) the following precautions are required:
- Exclusion of salt from the diet, to reduce the tendency to edema and ascites
- Moderation of the MA protein quota with a supplement of branched amino acids, since they do not require hepatic metabolization before cellular oxidation and have a very low level of nitrogenous waste (in turn responsible for the onset of hepatic encephalopathy). It is not possible to reduce too much the intake of amino acids since it would further alter the proteosynthesis of the liver; the consequent reduction of plasma proteins would determine: the collapse of oncotic pressure with a tendency to edema and ascites, and less coagulation capacity with the risk of bleeding
- Some authors suggest structuring a diet richer in energy than the normal one, that is, a HIGH-calorie diet. Personally I do not contest the choice but it is certainly necessary that these extra calories are mainly provided by glucose.