Depression: heterogeneous syndrome that alters the humoral stages of individuals at different levels, without real causes. Symptoms mainly involve the emotional-affective sphere, but neurodegenerative phenomena can also occur, such as mnemonic and talkative difficulties.
There are different types of depression:
- Depression reactive or secondary: due to serious contingent causes, such as real misfortunes.
- Depression endogenous: real pathology generally genetically determined, first treated with psychiatric therapy and then with drug therapy.
- Syndrome manic-depressive: bipolar affective disorder, which alternates stages of deep depression with stages of excessive and irrational euphoria; requires specific drug therapy.
The most probable cause of the onset of depression is a dysfunction in the central and peripheral transmission of neurotransmitters: norepinephrine, serotonin and dopamine; all of which are involved in the control of mood, sleep-wake cycle, appetite, "sexual activity and aggressive reactions. The alteration of these factors gives rise to the typical symptoms of depression.
There is an "etiological hypothesis for the onset of depression as a pathology, according to which the deficit of these neuroamines would cause the alteration of the functions they regulate. From this hypothesis two categories of drugs were born, MAO-inhibitors and TRICYCLES, with different mechanism of action, but the same pharmacological effect, ie the enhancement of noradrenergic and serotonergic transmission. These drugs have proved useful, but not sufficient: the "antidepressant effect appears after weeks of treatment, although neuronal transmission is restored a few hours after administration. The reason for this inconsistency is explained by the second hypothesis formulated by the scholars," neurotrophic hypothesis of depression; according to this theory, depression is caused not exclusively by the neuroaminergic deficit, but also by: alterations in the expression of the receptors of these neurotransmitters, alterations in the transduction mechanisms at the cytosol level and alterations during the gene expression of neurotrophic factors; the latter would cause phenomena of neuro degeneration, as they redefine the plasticity and neuronal survival. Second generation antidepressants tend to reduce these phenomena by inducing neurogenesis, that is, by restoring the function of damaged neurons; but even then it takes weeks of treatment before the effect takes place.
Classification of antidepressants.
- MAO inhibitors: irreversible inhibitors of mono-amino-oxidase, degradative enzymes of neuronal monoamines: this allows the neurotransmitters to be continuously released, without undergoing degradation. The first generation MAOIs are irreversible, while those of the second generation have some members with characteristics of reversible inhibitors and with fewer side effects than the first. However, they have limited use because they are hepatotoxic and require frequent administration and a diet low in tyramine-containing foods.
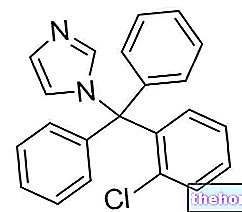
- Tricyclic antidepressants: For several years they have been the antidepressant drugs of first choice, as they are the most effective. The first was introduced in the 1950s and is able to block the transporters responsible for the reuptake of norepinephrine and serotonin at the synaptic level, therefore it induces an increase in the concentration of these neurotransmitters in an indirect way. These drugs against depression, however, have side effects. not negligible: they interact as antagonists of the muscarinic receptors of acetylcholine thus causing an inhibition of secretions, a reduction in gastric motility, water retention, blurred vision, tachycardia, CNS disorders (delusions, hallucinations ...); they always interact as antagonists of histamine H1 receptors causing drowsiness, weight gain, dizziness and central sedation; they also block noradrenergic α1 receptors causing vasodilation with consequent orthostatic hypotension, dizziness and sexual problems. These drugs also show a good affinity for heart tissue, generating cardiotoxicity; finally, they have a certain degree of tolerance, hence the need for a "gradual interruption.
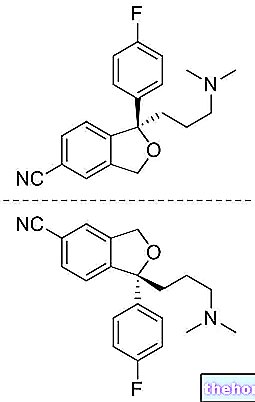
- Selective serotonin reuptake inhibitors (SSRIs): Discovered in the 1980s, they are able to selectively inhibit serotonin transporters; they do not interact with other noradrenergic receptors, therefore they do not have the side effects of tricyclics. classified according to their pharmacokinetics. The antidepressant effect is due to the increase of serotonin at the synaptic level; however this effect can carry secondary effects, such as: gastro-intestinal disturbances, sleep disturbances. In association with I-MAOs they can cause such an increase in the concentration of serotonin as to cause the so-called "serotonin syndrome", characterized by: tremors, muscle stiffness, mood swings, convulsions and coma Therapeutic dosages of SSRI antidepressants are effective and above all the most used, as they are easily administered.
- Selective norepinephrine reuptake inhibitors (NARI): pharmacological alternative to SSRIs, not equally effective.
- Specific serotonergic and noradrenergic antidepressants (NASSA): act as antagonists for the α2 receptors on nerve endings, physiologically responsible for blocking the release of serotonin and noradrenaline. Side effects are less severe, however there is a mild sedative state and a tendency to weight gain.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs): they have a multiple mechanism of action like the tricyclics, but without interacting with the M1, H1 and α1 receptors. The best known is the Duloxetnia, which inhibits the reuptake of both receptors in a balanced way; hence the need to administer low dosages; this drug against depression does not seem to have serious side effects, but the secondary effects related to renal function should be remembered: water retention and blocking of urination, currently being studied for the treatment of stress urinary incontinence.
- Hypericum perforatum: Hypericum or St. John's wort, used as an antidepressant; in vitro it was found that its inhibitory action on the reuptake of noadrenaline and serotonin is comparable to tricyclics or SNRIs. The methanolic or hydro-methanolic extract is effective for the treatment of mild or moderate depressions; however on the market there are many preparations based on hypericum, which is in fact also used as an antibacterial and anti-inflammatory for topical use. vegetable, hypericum has a high efficacy, therefore it is not recommended during pregnancy or breastfeeding, or in association with conventional antidpressants; moreover, it shows a high inducing effect of the hepatic microsomal system and a high photosensitivity. With reference to hypericum extracts, the bodies responsible for phytovigilance have reported photosensitivity, which can arise in case of excessive dosages but regresses after the interruption of the administration, and manic attacks (agitation, irritability, anxiety and insomnia).
More Articles on "Antidepressants, Depression Drugs"
- Depression - Drugs to Treat Depression
- Symptoms Depression
- Depressive disorders: major depressive episode
- Major depressive episode symptoms
- Dysthymic disorder
- Mania and manic episode
- Bipolar disorder
- Antidepressants
- Depression and hypericum
- Benzodiazepines - How do Benzodiazepines work?
- Pain: what does pain depend on?





















-nelle-carni-di-maiale.jpg)




