Curated by Doctor Ferdinando Spatalino
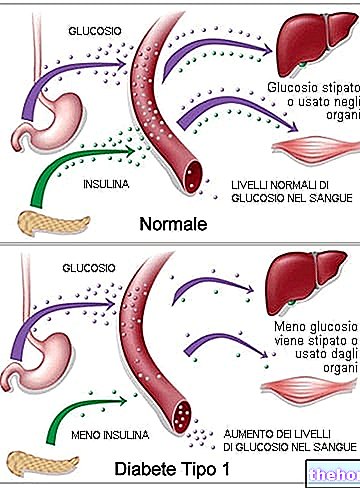
The term diabetes mellitus describes a metabolic disorder with multiple aetiology, characterized by chronic hyperglycemia with impaired metabolism of carbohydrates, fats and proteins, caused by defects in insulin secretion or insulin action, or both.
In common parlance there are two main forms of diabetes mellitus, called respectively type 1 or insulin-dependent diabetes and adult diabetes with insulin resistance or type 2.
Type 1 diabetes is autoimmune on a genetic basis; it affects young subjects up to 35 years of age and is determined by the destruction of the beta cells of the pancreas with consequent absolute insulin deficiency.
Type 2 diabetes, on the other hand, affects people over the age of 35 and at its origin there is a phenomenon called insulin resistance, a condition in which the ability of insulin to stimulate the uptake and utilization of glucose at the level of liver, skeletal muscle and adipose tissue, and to suppress the hepatic output of glucose. Type 2 diabetes may be present for a long time before the patient or doctor notices signs, as hyperglycemia and corresponding symptoms progress slowly. Among the young population it is increasing - possibly due to changing eating habits and increasingly sedentary lifestyle - another type of diabetes, MODY (Maturity Onset Diabetes of the Young), an early-onset type 2 diabetes.
Epidemiology
Diabetes is the most widespread and important metabolic disease present in Italy and in the Western world; it is estimated that the number of diabetics in Italy is about 3 million, to which must be added at least another 2 million cases not yet diagnosed. Against a prevalence of 3-5% of known cases, about 50% of cases of diabetes mellitus are in fact not yet diagnosed. Approximately 200,000 new cases occur each year, of which approximately 15,000 are type 1 and 185,000 are type 2.
Type 2 diabetes has a prevalence of around 5% in Western countries and an incidence of 23 new cases per 10,000 per year. These numbers still tend to increase according to what is published in the annual estimates of the International Diabetes Federation (IDF) and reported in the following table.

General economic impact and future prospects
The social impact of diabetic disease is of such magnitude, and the number of patients so high, that in many countries of the world, healthcare expenditure for this disease has reached 10% of global healthcare expenditure.
Costs in the United States have risen from $ 2.6 billion spent in 1969 to $ 98.2 billion in 1997, peaking at $ 137.7 billion in 1995. As far as Europe is concerned, the most important study is the Code-2 (Costs of Diabetes in Europe - type 2) created with the aim of estimating the costs of managing patients with diabetes in eight European countries (Belgium, France, Germany, Great Britain, Italy, Holland, Spain and Sweden). type 2. The American situation and the data reported by the Code-2 study for Europe are summarized in the graph in table 2. C "however, it should be noted that these studies do not take into account the overall value of the resources used for the treatment of complications , which far exceeds that of the resources for the treatment of diabetes. The average annual costs of the diabetic patient, respectively without complications (about 1100 euros), with only one type of complication (macrovascular: 3120 euros; microvascular: 4100 euros) and with all and two kinds of complicates nze (5650 euros), were clearly found to be a function of the complications themselves.

From the figures reported it is clear how important it is to support an increasingly widespread prevention campaign, in order to limit the growth of the disease: from studies carried out it appears that minimal interventions on lifestyle habits - such as physical activity, the adoption of a balanced diet and periodic monitoring of blood pressure and glycemic values - are able to delay the onset of type 2 diabetes by at least three years in 58% of subjects at risk.
Physical activity is therefore essential to keep the problem under control, improving the quality of life by about 50% and minimizing the risks that these imbalances cause to our physiological systems. Personal trainers become specialized in this area. therefore an obligation, given that the hypothetical customers to whom we all refer identify themselves according to the target of "Mrs. Maria", that is to say of any person who aims to improve their health through fitness. The "adjective" any "should not be understood in derogatory terms; rather, it refers to the possibility that our client is a carrier of various metabolic alterations, such as diabetes.
How does the personal trainer relate to the problem and how does he set up the training plan? First of all, it is necessary to have all the information regarding the case and, more importantly, to be clear about the problem from a physiological point of view; we must know that training a diabetic person involves changes in insulin action, that the time and intensity of training are not negligible factors, that just as there is a difference between type 1 diabetes and type 2 diabetes, there is also a different training approach etc.
In this regard, we refer to the reading of the following informative articles:
Physical activity and diabetes
Diabetes and exercise
Diabetes and circuit training
Obesity and personal trainer "