Key concepts
Purpura is a lesion similar to hematoma, a consequence of the rupture of capillaries under the surface of the skin. Petechial purpura (hematoma diameter <3 mm) is distinguished from ecchymotic purpura (lesion diameter between 1 and 2 cm).
Purpura: causes and classification
Purpura may or may not be related to thrombocytopenia.
- Thrombocytopenic purpura: may be caused by megaloblastic anemia, liver cirrhosis, leukemia, myeloma, idiopathic thrombocytopenic purpura, anticoagulant therapy, blood transfusion
- Non-thrombocytopenic purpura: can be caused by amyloidosis, micro-vascular damage, hemangioma, severe infections, hypertension, vasculitis, steroid drug therapy
- Purpura dependent on other coagulation disorders: disseminated intravascular coagulation, meningococcal meningitis, scurvy, splenomegaly
- Psychogenic purpura: dependent on emotional conditions
Purpura: diagnosis
Diagnosis is clinical and is based on medical observation of the lesions. A further diagnostic test is performed by biopsy.
Purpura: therapies
Treatment for purpura depends on the underlying causePurple: definition

Purple comes from the Latin term purpura, which means purple: the spots that appear on the skin due to trauma or disorders of the clotting capacity of the blood, in fact, have a purple or burgundy color, and do not discolour with acupressure.
Classification
Purpura can be classified on the basis of two important elements:
- Size of the hematoma
- Causes
Let's go step by step:
What types of purpura can be identified based on size?
- The small hematomas of the purpura (proper) have dimensions between 0.3 and 1 centimeter.
- The purple petechial (or simply petechiae) is characterized by small lesions, with a diameter of less than 3 millimeters.
- The purple ecchymotic (or bruising) precisely identifies more consistent lesions, with a diameter greater than 10 mm but less than 20 mm. Sometimes, ecchymotic purpura is difficult to distinguish from the actual hematoma (which, by definition, extends beyond 2 cm in size).
What variants of purpura exist based on the underlying cause?
Purpura is often caused by changes in the platelet count. People with thrombocytopenia are therefore at risk of developing small or large bruises on the surface of the skin or in the internal cavities.
Let us briefly recall that we speak of thrombocytopenia when the thrombocyte count (or platelets if you prefer) falls below 150,000 units per mm3.
Platelets, as we know, are very important constituents of the blood, which play a leading role in regulating haemostasis and maintaining the integrity of the vascular lining. When the number of platelets falls below the standard range, the regulation of coagulation capacity is lost.
Thus two groups of purpura are distinguished:
- Thrombocytopenic purpura: purpura is the expression of a more or less marked reduction in the number of platelets circulating in the blood.
The causes that reside in the appearance of this type of purpura clearly depend on what triggered the thrombocytopenia:
- MEGALOBLASTIC ANEMIA
- Taking drugs that prevent the formation of platelets (ANTICOAGULANT THERAPY)
- HEPATIC CIRRHOSIS: the number of platelets is reduced due to their destruction, induced by the disease
- LEUKEMIA: the reduction in the platelet count that characterizes this severe form of cancer predisposes the patient to ecchymosis, purpura, petechiae and hematomas.
- MYELOMA: neoplasm of the blood in which there is an uncontrolled production of cells of the immune system, used for the synthesis of antibodies.
- IDIOPATHIC THROMBOCYTOPENIC PURPLE: it is an autoimmune disease that is distinguished by the destruction of thrombocytes by auto-antibodies. Among the most frequent consequences, the appearance of red spots on the skin (purple) stands out. Thrombocytopenia neonatal autoimmune is a coagulation disease typical of babies born to mothers with ITP (autoimmune thrombocytopenia)
- BLOOD TRANSFUSION: there is a thrombocytopenia due to dilution
- NON thrombocytopenic purpura: The cause of purpura is not identifiable in the reduction of the platelet count. This variant of purpura results from vascular disorders, such as:
- AMYLOIDOSIS: disease characterized by the abnormal deposition of low molecular weight proteins in the extracellular area. The appearance of red spots on the skin (purpura, petechiae, ecchymosis) is a characteristic symptom of amyloidosis.
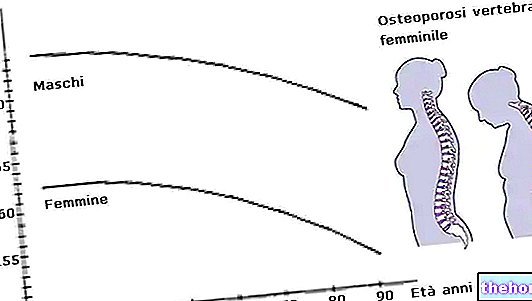
- MICRO-VASCULAR DAMAGES, typical of the elderly: advanced age makes the capillaries more fragile, therefore non-thrombocytopenic purpura is very frequent in the elderly. This form of purple takes on the connotation of actinic purpura, solar purple or senile purpura.
- CONNECTIVE DISORDERS: lupus erythematosus and rheumatoid arthritis
- HEMANGIOMA: this is an abnormal accumulation of blood vessels in the skin or internal organs. It is precisely a form of cancer in which blood vessels proliferate in the endothelium.
- SERIOUS INFECTIONS: Even serious infections can predispose the victim to the appearance of small red spots on the skin, including purpura. The most frequent infections are: smallpox, chicken pox, measles, Parvovirus B19 infections (fifth disease), Cytomegalovirus, rubella and meningitis.
- HYPERTENSION: a classic example is the pressure variations that occur during childbirth. Such a condition can favor the appearance of purpura in the parturient.
- VASCULITIS (inflammation of the blood vessels): Vasculitis is responsible for Henoch-Schönlein purpura (or anaphylactoid purpura). This variant of purpura is characterized by the accumulation of IgA, immune complexes originating from exposure to drugs, infectious agents or foods involved in airway infections.
- Therapy with STEROID DRUGS: taking corticosteroids for long periods can cause the onset of purpura, especially in the hands, arms and thighs. Steroid-dependent purpura is caused by the atrophy of the collagen fibers that support blood vessels. Clinical manifestations of steroid purpura are comparable to those of senile purpura.
An exaggerated consumption of saffron can cause toxic effects, even serious: among these, the bleeding induced by the reduction in the number of platelets (eg purpura) stands out.
- Bleeding dependent purpura: In addition to thrombocytopenia, other clotting disorders predispose to purpura.
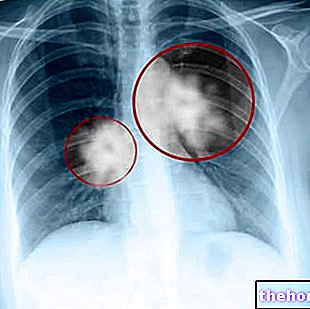
- Disseminated intravascular coagulation (typical consumption coagulopathy): this is a very dangerous disease characterized by the presence of thrombi (or clots) in the blood vessels. The abnormal and uncontrolled production of clots slowly consumes the coagulation factors; consequently, the blood has a low propensity to clot, therefore it triggers hemorrhagic phenomena (purpura and more serious lesions).
- Meningococcal meningitis (Neisseria meningitidis)
- Scurvy (severe vitamin C deficiency disease): the walls of the blood capillaries are fragile and weakened, therefore the affected patient has petechiae, purpura and bruising throughout the body.
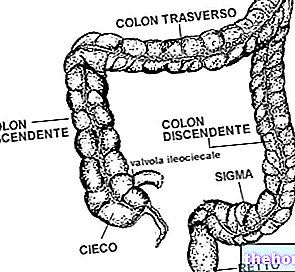
- Splenomegaly: the increase in volume of the spleen can alter the clotting capacity of the blood, sequester platelets and favor the formation of red spots on the skin (purpura).
- Psychogenic purpura: according to some authors, there is also a psychogenic form of purpura. Under certain conditions, the typical red flecks of purple tend to accentuate in response to emotional conditions of stress, tension or anxiety. Psychogenic purpura occurs more frequently in middle-aged women with a particularly unstable personality, predisposed to epitaxis or other hemorrhages. Psychogenic purpura is best described in the literature by the term ".Gardner-Diamond purple'.
Diagnosis and therapies
The diagnosis for purpura is essentially clinical, therefore it is based on direct medical observation of the lesions. Eventually, for a diagnostic assessment, it is possible to undergo a skin biopsy. Treatment for purpura depends on the triggering cause:
- Antibiotics are recommended for bacterial infections
- Antiviral drugs are indicated for the treatment of virus-dependent purpura
- Scurvy-dependent purpura is treated by taking vitamin C
- Patients predisposed to the so-called psychogenic purpura should take relaxation courses or take antidepressant / anxiolytic drugs (subject to medical prescription)
- For purpura dependent on severe platelet reduction: read the article on drugs to treat thrombocytopenia
- For purpura caused by spleen enlargement: read the article on drugs to treat splenomegaly
Patients with impaired blood clotting capacity should avoid intramuscular drug administration, and prefer the intravenous route; by doing so, the risk of developing bruising, purpura, petechiae and hematomas is minimized.