Causes
The precise cause of uterine polyposis is unknown. S "hypothesizes that the development of polyps in the uterus depends on the excessive growth of endometrial cells, linked to estrogenic alterations. Women aged between 40 and 50 years (pre-menopausal period) are more exposed to the risk of uterine polyposis.

Symptoms
When symptomatic, the presence of the uterine polyp must be assumed in the following cases: irregular menstrual cycle, dysmenorrhea, hypermenorrhea, menorrhagia, spotting.
Diagnosis
Diagnosis of uterine polyposis can be ascertained by transvaginal ultrasound examination, curettage, diagnostic hysteroscopy, or hysterosalpingography.
Therapy
Benign and small uterine polyps do not need any specific treatment. Sometimes, drug therapy (progestogens or gonadotropins) may be required. Large uterine polyps must be surgically removed (therapeutic hysteroscopy or hysterectomy).
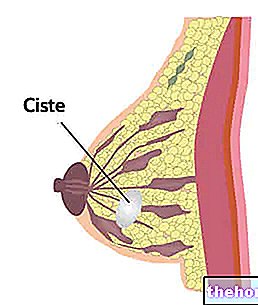
Uterine polyps consist of a tissue rich in mucous glands. By increasing in volume, the tissue - already extremely fragile and delicate in itself - can cause bleeding, sometimes very copious.
The size of uterine polyps varies from a few millimeters to a few centimeters. They can grow singly, in pairs, or form larger groups (complex aggregates consisting of many small polyps).
Uterine polyps can be classified according to how they are anchored to the wall of the uterus:

- Pedunculated uterine polyps: they are fixed to the uterine mucosa by means of a peduncle. More often than not, these growths remain confined to the inside of the uterus; however, although rarely, they can protrude into the vagina
- Sessile uterine polyps: they are anchored to the uterine mucosa with their entire base and, not being pedunculated, they cannot protrude into the vagina.
Uterine polyps can appear in women of any age, therefore they develop both during the woman's fertile period and after menopause (rare). In any case, the peak incidence is recorded in the age between 40 and 50 years, while it is rare that the phenomenon affects adolescents.
: in fact, uterine polyps are estrogen-sensitive, that is, they respond to estrogen similarly to the endometrium.Among the risk factors for uterine polyposis we remember:
- Age between 40 and 50 years
- Genetic predisposition
The clinical symptoms of uterine polyps are not very evident: many women do not perceive the presence of a polyp until they undergo a standard gynecological examination.
However, uterine polyps are prone to bleeding, so abnormal uterine discharge - outside of the menstrual cycle - can be a warning sign of a uterine polyp.
When symptomatic, uterine polyps can cause different discomforts:
- Irregular menstrual cycle
- Dysmenorrhea (painful menstruation) accompanied by severe abdominal cramps
- Dyspareunia (pain during sexual intercourse)
- Hypermenorrhea (heavy periods) or menorrhagia (extremely profuse blood loss during menstruation)
- Menstruation-like uterine discharge during the postmenopausal period
- Spotting
A polyp can create complications when it grows near the fallopian tubes, particularly when its size is important. In such circumstances, in fact, the uterine polyp can obstruct the tube openings, hindering fertilization and becoming a possible cause of infertility.
- Most uterine polyps constitute a benign condition: the probability of degeneration into tumor forms is very low.
Uterine polyps can also be diagnosed by scraping (or curettage): the tissue sample taken will be subsequently examined in the laboratory to exclude a possible malignant lesion. Hysteroscopy is also sometimes performed to confirm a suspicion of a uterine polyp: this technique uses a special instrument (hysteroscope) to view the interior of the uterine cavity. The hysteroscopy diagnostics it constitutes a "fundamental investigation in the differential diagnosis of the various causes of menstrual alteration (including uterine polyposis).
Last but not least, hysterosalpingography, a radiological test useful for assessing the state of health of the uterus and fallopian tubes. Medicines for the treatment of uterine polyps
Small-sized benign uterine polyps tend to self-resolve over a short period, although it is advisable to keep them under control to avoid a possible (although unlikely) neoplastic evolution.
There is also a drug therapy for the treatment of uterine polyps. However, taking progestins or gonadotropins is not the best choice for eliminating uterine growths, since the risk of recurrence is very high.
Although it is an almost harmless and benign condition, large uterine polyps must be treated surgically, since they can create significant menstrual discomfort.
The therapy consists in the "exeresis of the polyp, or in its surgical removal:
- Hysteroscopy (therapeutic): consists in the complete surgical removal of the uterine polyp
- Hysterectomy (removal of the uterus): indicated when the uterine polyps contain malignant neoplastic cells
Even after a perfectly successful surgical treatment, uterine polyps tend to recur. In the event of a relapse, the woman will have to undergo further surgery.