Dyspareunia is included among the Female Sexual Disorders (Female Sexual Dysfunctions, FDS) and is often associated with vaginismus and other non-coital sexual disorders; if vaginismus is a generally occurring disorder first of sexual intercourse and consists in the phobia of penetration, pain in dyspareunia coincides with the sexual act.

(as well as "negative" stress) could be mild, medium or severe, and affect dyspareunia differently.
An in-depth study will be devoted to these last two parameters (nature of the causes and localization of pain), given their considerable impact on dyspareunia.
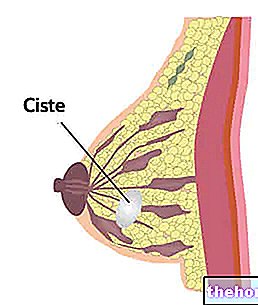
dyspareunia: a correct analysis of the causes is useful for the doctor to grasp the peculiar aspects of the disease; consequently it will be easier to diagnose e cure dyspareunia.As already mentioned, dyspareunia can be introital (or superficial), mid-vaginal or deep: although superficial and mid-vaginal dyspareunias are both perceived by the woman in the preliminary stage of intercourse, the two types are linked to different causal factors, although presenting many similarities. On the other hand, with regard to profound dyspareunia, both the symptoms and the causes are well differentiated from the previous ones.
The substantial difference between mid-vaginal and superficial dyspareunia lies in the "defensive" contraction of the levator anus muscle, typical of mid-vaginal dyspareunia and absent in the superficial. Both the aforementioned types of dyspareunia may be related to causes of a psychosexual nature, biological and relational.
- Psychosexual causes are favored by libido disorders, sexual harassment and violence, anxiety and depression. Often, three psychosexual causes that favor dyspareunia, coexist multiple sexual disorders such as, for example, vaginismus, decreased arousal, loss of desire, etc. Dyspareunia could also be triggered by some episodes of childhood: women who have been subjected to rape or sexual violence when they are young tend to complain of disorders of a sexual nature even in adulthood and dyspareunia falls into this category.
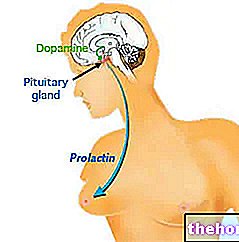
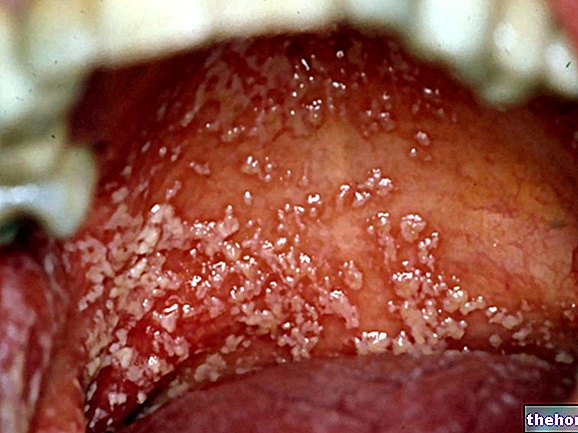
- The biological triggers that affect superficial and mid-vaginal dyspareunia can be infectious, hormonal, iatrogenic (caused by drugs), vascular, muscular and connective. Vaginal infections, such as candidiasis, could greatly affect pain on penetration: Candida, in addition to causing dyspareunia, causes a known decrease in libido and arousal which is sometimes also reflected in the partner.
- By "relational causes" we basically refer to a decrease in libido, problems with the partner and a marked sexual dissatisfaction.
Vulvar vestibulitis - inflammation affecting the clitoris, vaginal entrance and urethral orifice - certainly represents the prevalent etiological factor that predisposes to superficial and mid-vaginal dyspareunia.
Among the factors that cause profound dyspareunia, endometriosis, the syndrome, stands out by entrapment of the abdominal nerves, pelvic varicocele and PID (pelvic inflammatory disease): the causes listed above are considered biological factors, which can add up to other causative elements and make intercourse even more painful.
certainly do not help to resolve dyspareunia. Rather, the history of each individual patient must be scrupulously studied in order to bring dyspareunia to remission.
pelvic and PID (pelvic inflammatory disease)Symptomatology
The pain caused by intercourse may persist even a few days after having consummated intercourse;
in addition: vaginal dryness, alteration of vaginal pH, intolerance to the use of internal tampons during the menstrual cycle, and perception of pain even during gynecological check-ups
Single and couple psychological therapy is probably the best solution




















-nelle-carni-di-maiale.jpg)




