Scroll down to read the summary table on dyskinesia
- Dystonia: involuntary muscle contractions, protracted over time, characterized by repetitive and cadenced gestures
- Akathisia: internal tremor
- Tardive dyskinesias: collateral dyskinesia typical of the administration of antipsychotic-neuroleptic and antiemetic substances. Characterized by involuntary hyperkinetic movements, stiffness, muscle tension, bradykinesia, stereotyped, frequent and rhythmic movements
- Tardive withdrawal dyskinesia: hyperkinetic movements follow the interruption of drug therapy
- Athetosis: involuntary movements are particularly slow
- Korea: movements appear rapid, continuous and uncontrolled
- Cramps: the movements are involuntary and painful, the cause of which lies above all in the excessive muscular effort
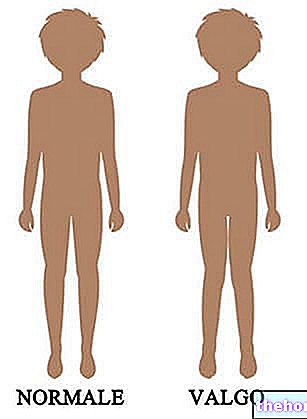
- Dystonia: abnormal posture assumed by the body
- Hemiballism: particularly violent movements of the body
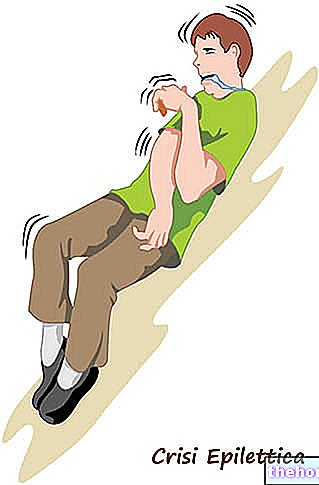
- Myoclonus: short and temporary involuntary movements typical of sleep
- Synkinesia: involuntary movement with one limb, when the movement is being made in the other limb
- Tics: repeated, identical and rhythmic movements (psychogenic nature)
- Tremors: rhythmic muscle oscillations not predicted by the CNS, generated by antagonistic muscle bundles
- uterine dyskinesia
- biliary dyskinesia
- myocardial dyskinesia
- dyskinesias of the upper esophageal sphincter
- primary ciliary dyskinesia
- Hyperkinesias
- Hypokinesias
Psychological consequences: possible psycho-social disturbances, mentally incapacitating
General clinical picture:
- Facial and eye movements
- Perioral dyskinesias
- Movements of the extremities
- Trunk dyskinesias
- Constant and chronic administration of neuroleptic-antipsychotic drugs used in the treatment of depression, nausea and dyspepsia
- The risk of causing dyskinesia is directly proportional to the increase in dosage and duration of treatment.
- Aging of the patient
- Probably, women are more at risk, particularly during the menopausal period
- Depression, degenerative diseases (eg diabetes) and Parkinson's disease
- Smoking, alcohol and drugs
- Possible genetic predisposition
- Multidisciplinary approach
- Clinical-objective examination of the patient: control of all hypokinetic or hyperkinetic movements of the patient
- Psycho-neurological analysis of the patient
- AIMS scale: investigation tool useful for recognizing the initial symptoms of dyskinesia and for monitoring any pathological degeneration over time
- Laboratory tests (e.g. SMA-18, CBC, etc.)
- Family history (to verify hypothetical diseases of neurological origin)
- Reduction of the dosage of neuroleptic substances for patients who still have psychotic disorders
- Discontinuation of the drug when the patient has completely recovered from the psychosis
- New possible effective therapeutic options: vitamin D, botulinum toxin and tetrabenazine
Replacement of the neuroleptic drug with another, with fewer side effects on muscle movement
Other articles on "Dyskinesia in brief: summary of dyskinesia"
- Dyskinesia: Diagnosis, Therapy, Prevention
- Dyskinesia
- Dyskinesia: clinical picture and risk factors