As we know, celiac disease represents a "permanent intolerance to gluten, an autoimmune disease, ambiguous and equivocal, which manifests itself in various ways, leading to consequences such as abdominal swelling, colitis, flatulence, osteoporosis and oral aphthosis.
Erroneously, dermatitis herpetiformis tends to be considered an autoimmune disease; considering, however, the ascertained correlation with celiac disease, Duhring's dermatitis is more correctly classified as a cutaneous manifestation of a "food intolerance.
In addition to this, even the "herpetiform" name can be misleading: in fact, at first glance, one might think that this form of dermatitis has a certain connection with the infections triggered by Herpes simplex. In reality there is "no etiopathological correlation with the"Herpes: the term herpetiform has in fact been attributed for the particular manifestations of this dermatitis, with the appearance of particular blisters, bubbles and crusts, which recall the typical signs left by the aforementioned virus.
The wording "Duhring's", on the other hand, is due to the doctor who identified and described the disease, for the first time, in 1884. Later, in 1988, the disease in question was also clinically described by Brocq (hence the name of "Brocq's painful polymorphic dermatitis").
However, to identify the close relationship between this disease and the celiac manifestation, it was necessary to wait until 1966.
, with an "incidence of one person in 10,000; Ireland is an" exception, as the disease occurs with a frequency of 1: 500.
Dermatitis herpetiformis occurs in young people and adults and it is very rare for dermatitis herpetiformis to affect infants and the elderly.
It is particularly widespread in Caucasian celiac individuals in Northern Europe; while it rarely affects people of Asian or black ethnicity.
Although rare in infants, dermatitis herpetiformis can manifest its first symptoms in adolescence, with greater incidence in females. On the contrary, in adulthood it is male individuals who are most affected.
Statistics also link dermatitis herpetiformis with celiac disease: the skin disorder occurs in every five people with celiac disease. In fact, not necessarily all celiac individuals also suffer from this skin disease. Conversely, an individual with Duhring's dermatitis will surely have celiac disease.
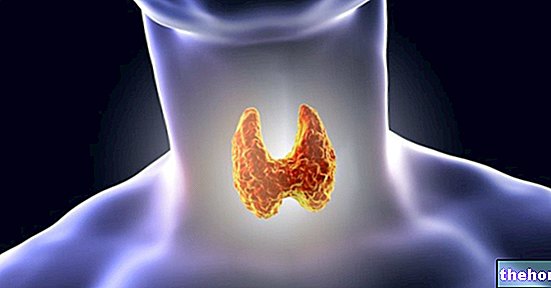
: gluten is the cause of the abnormal antibody response (IgA - type A immunoglobulins) responsible for the dermal manifestation.On the other hand, it is true that the herpetiform manifestation is often associated with other auto-immune pathologies (pernicious anemia, type 1 diabetes or thyroid disorders).
The genetic footprint and predisposition, in any case, always play a role of primary importance in the etiopathogenesis of dermatitis herpetiformis: both this dermal manifestation and celiac disease, therefore, demonstrate the same genetic sensitivity (the genes involved are the same) and, in both diseases, gluten is responsible for the autoimmune reaction.
Immune reactions are controlled by the antigen identification system called HLA (Human Leukocyte Antigen), fundamental for the correct functioning of defense systems: when the genes that control this system are altered, the probability that the subject is affected by one or both diseases is very high; celiacs, in particular, generally have a specific HLA gene.
To better understand: as a consequence of a genetic predisposition and its interaction with other unrecognized factors, both in the herpetiform manifestation of Duhring and in celiac disease, we are witnessing a failure to recognize some structures of the organism by the immune system. dermatitis herpetiformis antibodies attack the skin causing damage to the keratinocytes (skin cells), while in celiac disease the attack occurs in the intestinal mucosa.
, accompanied by irritation and inflammation: the course is certainly not natural, since it is the immune system itself that generates the reaction.Generally, the appearance of rashes is preceded by severe itching or burning sensations that often occur in the elbows, knees, lower back and even in the scalp.
Dermatitis can progress and manifest small blisters and blisters: the damage to the skin, however, does not remain unnoticed, as the subject is continually subjected to a ferocious and unbearable itch, so much so that he cannot resist the urge to scratch and rub the interested party continuously. By doing so, skin irritation worsens exponentially, blisters and blisters burst resulting in the formation of scabs, ulcers, erosions and scars. In some cases, even small bleeding can occur.
The rash progresses slowly but inexorably: at first small blisters appear scattered in specific areas of the body, which then evolve into more severe forms, sometimes even affecting the entire body surface; the sites most affected by herpetiform dermatitis are the legs, arms and back, although there are also possible rashes on the face and scalp.
When the scabs disappear, the scars remain: in these points, the skin could undergo chromatic variations (hypo-pigmentation or, more rarely, hyper-pigmentation) compared to the uninjured skin.
In rare cases, the disease may regress until it finally disappears.
In the majority of cases, moreover, individuals suffering from herpetiform dermatitis also manifest intestinal symptoms, such as diarrhea and abdominal pain which tend to increase with the ingestion of foods containing gluten, precisely because of the direct correlation with celiac disease.
") or eczema. The patient must immediately go to a specialist, who will have to perform a biopsy (invasive examination that involves the removal and analysis of a part of the tissue), associated with the search for the antibodies that have triggered the problem, in order to shed light on the " origin of the disease. A small piece of skin tissue not injured it is taken and analyzed: if the analysis is positive in the presence of specific IgA, then the patient is probably considered to have Duhring's dermatitis.IgA are antibodies that belong to the immune system: in the intestine, type A immunoglobulins are essential for protection from attacks by pathogenic microorganisms; if the IgA binds to particular skin tissues, dermatitis can be triggered, as the cells of the immune system rebel against the organism itself.
A further diagnosis is made through blood tests: the antibodies responsible for gluten intolerance are also searched for in the blood. Among the antibodies that are identified we remember: the antiendomysium, anti-gliadin, and tissue antitransglutaminase antibodies.
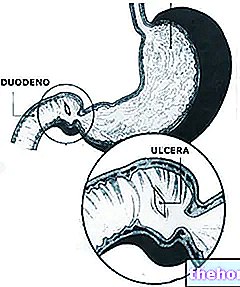
Celiacs show atrophy of the intestinal villi, associated with folic acid and iron deficiency: the same conditions are found in subjects suffering from herpetiform dermatitis, therefore it is advisable to search for any deficiencies of these substances for the in-depth diagnosis of dermatitis.
The assessment of the disease is absolutely essential: if a precise diagnosis has not been conducted, it is not possible to proceed with a resolutive therapy.
containing gluten.
A gluten-free diet is, in fact, the only possible treatment, capable of completely eradicating the triggering factors.If this is not enough, with the advice of the doctor, it is possible to resort to the use of specific drugs.
Pharmacological treatment
If the gluten-free diet is not sufficient to prevent the onset of dermatitis herpetiformis, the doctor may prescribe the patient to take certain drugs in order to counteract the symptoms of the disease.
In this regard, the active ingredients usually used are dapsone (preferential therapy) and sulfapyridine (alternative treatment less effective than the previous one).
Generally, these drugs act rather quickly, so much so that - in most cases - the symptoms resolve after a few days of treatment.
These powerful drugs, however, can cause secondary side effects such as vomiting, anemia and lack of appetite. Furthermore, they act only in the skin manifestation, not reporting any efficacy in the intestine (they are not suitable for counteracting celiac disease).
To conclude, therefore, only a scrupulous gluten-free diet represents the most appropriate solution to counteract the onset of dermatitis herpetiformis.