Administrable through different routes (oral, transdermal, parenteral), clonidine is used in the treatment of hypertension and hypertensive crises. Medicines containing clonidine that can be administered orally and transdermally can be dispensed in pharmacies upon presentation of a repeatable medical prescription ( RR); some of them are classified as class A drugs, therefore, their cost can be reimbursed by the National Health System (SSN); others, on the other hand, are classified as class C drugs, therefore, their dispensing takes place at full charge. On the other hand, clonidine-based medicines suitable for parenteral administration are for hospital use only.
Examples of Medicines containing Clonidine
- Catapresan®
- Catapresan TTS® (transdermal patches)
- Clonidine Hydrochloride Bioindustria L.I.M.®
Parenterally administered clonidine, on the other hand, is indicated in the treatment of hypertensive crises and in cases where it is temporarily not possible to administer the drug by mouth, or when administration by mouth has not proved effective enough. In any case, the parenteral route is reserved for hospitalized patients.
recent;Also, before taking clonidine medicines, it is important to know that:
- During the first week of treatment, clonidine can cause sedation which usually subsides with continued therapy. However, if necessary, your doctor can decrease the amount of medicine administered.
- Clonidine treatment should be discontinued gradually and only under close medical supervision.
- Clonidine can cause reduced lacrimation, patients wearing contact lenses should be informed.
- Patients who have experienced local skin reactions following the use of the clonidine-based transdermal patch may develop widespread rash on switching to oral therapy.
- When using clonidine-based transdermal patches, you should contact your doctor to consider removing the patch in the event of moderate to severe localized erythema and / or application site blistering, or a "skin rash" generalized type.
Note: If "local, isolated, minor skin irritation is observed within 7 days of applying the patch, it can be removed and replaced with a new one, applied to another" skin area.
Precautions for using the transdermal patch
- Use of the clonidine transdermal patch should not be discontinued during the surgical period. Blood pressure should be closely monitored during surgery and additional pressure control measures should be available if needed.
- When considering initiation of therapy with the clonidine-based transdermal patch during the perioperative period, it should be considered that therapeutic plasma levels are not reached until 2-3 days after initial application.
- The transdermal patch must be removed before defibrillation or cardioversion operations due to the potential alteration of electrical conductivity, which can increase the risk of arcing, a phenomenon associated with the use of defibrillators.
- Since the clonidine-based transdermal patch contains aluminum, it is recommended to remove it before undergoing magnetic resonance imaging (MRI). Skin burns at the patch application site have been reported in numerous patients who wore an aluminum-containing transdermal patch during magnetic resonance imaging (MRI).
Please note
- The use of clonidine is NOT effective in the treatment of pheochromocytoma hypertension.
- The use of clonidine in children and adolescents is NOT recommended.
- Serious adverse reactions - including death - have been reported in the off-label use of clonidine in combination with methylphenidate in children with ADHD, therefore, this combination and use are absolutely NOT recommended.
- Undesirable effects such as dizziness, sedation and disturbances in accommodation may occur during treatment with clonidine. Extreme caution is recommended when driving and operating machinery and avoiding such activities should such effects occur.
In light of the above, it is absolutely important to inform your doctor if you are taking one or more of the aforementioned drugs or substances (alcohol). In any case, the doctor should be informed if you are taking, have recently taken or intend to take any kind of medicines or products, including non-prescription drugs (SOPs), over-the-counter drugs (OTC), herbal and phytotherapeutic products and homeopathic products.
, manifesting undesirable effects different in type and intensity, or not manifesting them at all.
Very common and common side effects
Among the undesirable effects that most commonly may arise during treatment with clonidine, we find:
- Dizziness;
- Sedation;
- Orthostatic hypotension;
- Dry mouth
- Depression;
- Sleep disorders;
- Headache
- Constipation;
- Nausea and / or vomiting;
- Pain in the salivary glands
- Fatigue and erectile dysfunction.
Uncommon side effects
Uncommon side effects that may occur during clonidine therapy include:
- Hallucinations;
- Delusional perception;
- Nightmares
- Paresthesia;
- Sinus bradycardia;
- Raynaud's syndrome;
- Itching, rash, hives;
- Malaise.
Rare side effects and of unknown frequency
Among the undesirable effects that can occur more rarely when taking clonidine, however, we find:
- Gynecomastia;
- Reduction of tear flow;
- Atrioventricular block;
- Dryness of the nasal mucosa;
- Pseudo-obstructions of the large intestine;
- Alopecia;
- Increased blood sugar;
- Disorders of accommodation;
- Bradyarrhythmias.
Clonidine overdose
Clonidine overdose can cause symptoms such as:
- Constriction of the pupil;
- Lethargy
- Bradycardia;
- Hypotension;
- Hypothermia;
- Somnolence up to coma;
- Respiratory depression tending to apnea;
- Paradoxical hypertension.
Emergency treatment consists of gastric lavage and the administration of analeptic and / or vasopressor drugs.
In case of ingestion / intake of an excessive dose of clonidine, you must notify your doctor immediately or go to the nearest hospital.
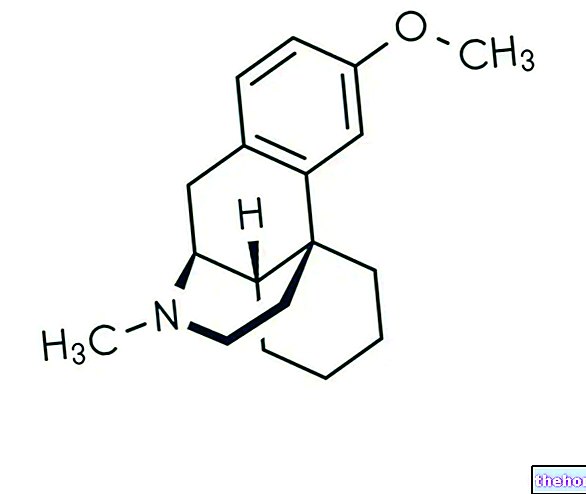
which results in a decrease in peripheral and renal resistance, a reduction in blood pressure and heart rhythm. All this is possible thanks to the agonist action of the α2-adrenergic receptors that the active principle exerts. who are more sensitive to the drug: 75-150 micrograms of clonidine per day (corresponding to ½ tablet - 1 tablet of 150 mcg), preferably in the evening. In case of insufficient response, the doctor may increase the amount of medicine administered up to 450 micrograms per day (corresponding to 3 tablets of 150 micrograms).Transdermal clonidine
Clonidine-based transdermal patches are available in three variants: patches containing 2.5 mg of active substance (TTS-1), patches containing 2.5 mg of active substance (TTS-2) and patches containing 7.5 mg of active principle.
Usually, treatment starts with a 2.5 mg transdermal patch, after which the dose will be adjusted by your doctor until the desired effect is achieved.
If after 1 or 2 weeks the reduction in blood pressure is not sufficient, the dosage can be increased by adding another 2.5 mg patch, or by using the 5 mg patch. An increase in dosage above two 7.5 mg patches is not usually accompanied by an increase in efficacy.
Please note
When the transdermal patch is applied for the first time as a replacement for oral therapy with clonidine or other antihypertensive medicinal products, it is necessary to be aware that the antihypertensive effect exerted by clonidine in the transdermal patch may not be achieved before 2-3 Therefore, it is advisable to gradually reduce the dosage of the medicine in use and not to stop suddenly. Some or all of the previous antihypertensive therapies may however be maintained, especially in patients with more severe forms of hypertension. The doctor will inform the patient on how to behave and how to gradually reduce the dosage of drugs.
To apply the patch, follow the instructions provided by your doctor and those reported on the package leaflet of the medicine.
Clonidine parenterally
The use of parenteral clonidine is reserved for hospitalized patients for the treatment of hypertensive crises or in those patients in whom oral administration is not possible or has not given adequate results.
Clonidine can be administered by subcutaneous or intramuscular injection, or by slow intravenous route.
Stop taking Clonidine
Any suspension of treatment must take place exclusively under medical supervision and gradually with graduated doses, over a few days, in order to avoid a consequent sudden increase in blood pressure with the classic symptoms (agitation, palpitations, nervousness, tremor, headache, nausea, etc.).
If it is necessary to discontinue concomitant long-term β-blocker treatment, the β-blocker should be discontinued several days before the gradual withdrawal of clonidine.
and can reduce the heart rate of the fetus, careful and continuous monitoring of the mother and fetus is essential. After delivery, however, there may be a transient increase in the blood pressure of the newborn.
If necessary, oral therapy with clonidine is preferred during pregnancy, while parenteral therapy should be avoided. In any case, the doctor will decide if, how and when to administer the active ingredient.
Clonidine is excreted in breast milk and there are insufficient data on the effects of the active substance on the newborn. Therefore, the use of clonidine in breastfeeding mothers is not recommended.