" bronchial asthma
Doctor-Patient Relationship
Sensitize the patient to develop a close collaboration relationship with the doctor
The management of asthma requires the development of a close relationship between the asthmatic patient and the physician.
With the help of the physician, patients should learn to:
- Avoid exposure to risk factors.
- Take medications correctly.
- Understanding the difference between "background" anti-asthma drugs, to be taken continuously, and "reliever" drugs, to be taken only when there is a real need.
- Monitor health by interpreting symptoms and, if possible, measure peak expiratory flow (PEF).
- Recognize the warning signs of asthma attacks and take appropriate action.
- Seek immediate medical attention in case of need.
The education of the asthmatic patient should therefore be an integral part of the doctor-patient relationship. With a series of methods - such as interviews (with the doctor and nurses), demonstrations and written material - it is possible to reinforce the messages educational.
Healthcare professionals should prepare in writing, with the patient, an individual, correct and understandable treatment program that the asthmatic person can actually carry out.
Medicines and Treatment
Drugs to be used as needed
Symptomatic drugs are identified:
- in beta2-agonists
- in anticholinergics.
Based on the duration of the bronchodilating effect, beta2-agonists are divided into active ingredients
- short-acting: salbutamol And terbutaline
- long-lasting action: salmeterol And formoterol.

For this reason they are NOT considered first choice bronchodilator drugs in the treatment of bronchial asthma.
Fund drugs
The purpose of the drugs used in background therapy is to keep the disease under control, i.e. in the absence of symptoms. Their activity is aimed at reducing the bronchial inflammatory process, which begins very early, thus making the subject asymptomatic. The most effective drugs are:
- inhaled corticosteroids (beclomethasone, budesonide, flunisolide, fluticasone, mometasone),
- chromones (sodium chromyl, sodium chromoglycate),
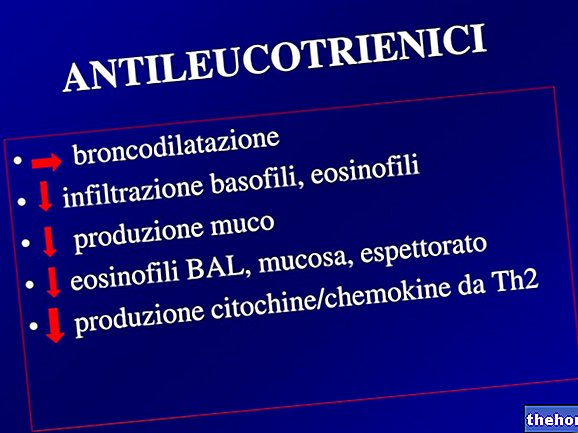
- antileukotriene for their ability to inhibit phlogogenic mediators and inducing bronchial spasm.
Therapeutic setting
The therapeutic approach depends on the clinical-functional status.
Critical period
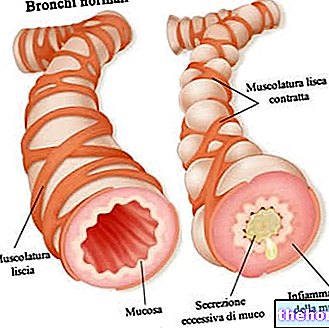
In the critical period, to reduce the particularly active inflammatory state, and bronchostruction, it is necessary to combine anti-inflammatory drugs and beta2-agonists, in order to restore, in a short time, the bronchial patency to a level that allows the resumption of normal daily activity .
Serious forms
In the more marked forms, on the other hand, the use of high-dose corticosteroids, associated with salmeterol or formoterol for their long-lasting action, is recommended.
Mild forms
In the milder forms, the use of chromones, or corticosteroids, at lower doses, associated or not with salbutamol or terbutaline according to need, has proved very useful.
Treatment must be continued with both drugs (anti-inflammatory and bronchodilator) until the clinical-functional picture stabilizes at the level prior to the crisis. Once this goal has been reached, it is necessary to continue with anti-inflammatory therapy alone for a suitable period of time, as the inflammation of the airways can persist for long periods.
Intercritical period
In the intercritical period, when the subject is clinically asymptomatic, the need or not for pharmacological treatment is given by the functional condition detected with spirometry. If the data are normal, no therapy is required; if, on the other hand, there is an obstructive picture (albeit asymptomatic) it is necessary to set up a long-term therapy with inhaled corticosteroids and, possibly, long-acting beta2-agonists. In seasonal allergic subjects it is advisable to start a pharmacoprophylaxis with anti-inflammatories a few weeks before the presumed critical period based on allergic tests.
Also in the intercritical period, it is essential to evaluate the bronchial hyperreactivity of the asthmatic patient with an exercise test, in order to verify the existence of exercise-induced bronchospasm - often limiting sports performance - hence the need to establish an "adequate pharmacoprophylaxis. . This is based on beta2-agonist drugs in combination or as an alternative to chromones (although the latter may be less effective), to be administered before performance
Even antileukotrienics, used for the treatment of acute episodes, but above all taken for prolonged periods of time, have shown an "effective preventive action.
Prevention
To improve asthma control and reduce the need for reliever medications, patients should avoid exposure to the risk factors that trigger asthma symptoms.
Physical activity is a stimulus that can trigger asthma symptoms, but patients should not avoid exercise. Symptoms can be prevented by taking a fast-acting drug as needed, before beginning strenuous physical activity (alternatives are antileukotrienes or chromones).
Patients with asthma of moderate severity should undergo flu vaccination annually, or at least for as long as vaccination in the general population is recommended. Influenza vaccines with inactivated viruses are safe for adults and children over 3 years of age.
Conclusions
Bronchial asthma is responsible for a high consumption of health resources, both in terms of direct costs for the management of the disease - consisting of costs for drugs, for health services and hospitalizations of the most serious cases - and in terms of costs indirect, linked to lack of productivity due to absences from work or school and poor quality of life.
The results of recent research show that there is still a diagnostic delay due both to the initial lack of motivation of patients to go to the doctor - to report on the presence of symptoms, relying more on the transience of the problem and on self-medication - and uncertainty. of the doctor to subject his client to a spirometric examination to confirm the diagnostic suspicion for asthma.
This behavior causes a delay in the definition and regularity of the antiasthmatic therapy; in the meantime, there is insufficient control of the disease and a persistence of limitations in the patient's relational life, which are often unjustified, as most asthma patients are able to achieve and maintain physical well-being close to, if not equal to, non-asthmatic subjects .
It is therefore necessary to draw the attention of health personnel to the importance of a correct management of this frequent disease.
Bibliography:
- World Asthma Project - www.ginasma.it
- Barbara P. Yawn, Paul L. Enright, Robert F. Lemanske, Jr, Elliot Israel, Wilson Pace, Peter Wollan, and Homer Boushey
Spirometry Can Be Done in Family Physicians "Offices and Alters Clinical Decisions in Management of Asthma and COPD.
Chest Oct 2007: 1162 - 1168 - Barnes PJ.
Scientific rationale for using a single inhaler for asthma control.
Eur Respir J 2007; 29: 1-9. - Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007.
J Allergy Clin Immunol. 2007 Nov; 120 (5 Suppl): S94-138. - Masoli M, Williams M, Weatherall M, et al.
The 24 h duration of bronchodilator action of the budesonide / formoterol combination inhaler.
Respir Med 2006; 100: 20 - 5 - Navarro RP, Schaecher KL, Rice GK:
Asthma management guidelines: updates, advances, and new options.
J Manag Care Pharm. 2007 Aug; 13 (6 Suppl D): S3-11; quiz S12-3. - Partridge M, van der Molen T, Myrseth S-E, et al.
Attitudes and actions of asthma patients on regular maintenance therapy: The INSPIRE study.
BMC Pulm Med 2006; 6:13. - Rabe KF, Atienza T, Magyar P, et al.
Effect of budesonide in combination with formoterol for reliever therapy in asthma exacerbations: a randomized controlled, double-blind study.
Lancet 2006; 368: 744 - 53.
Other articles on "Bronchial Asthma - Treatment, Drugs and Prevention"
- Bronchial asthma
- Asthma
- Asthma - Asthma Treatment Drugs
- Diet and Asthma
- Asthmatic Crises (Asthma Attacks)
- Anti-asthmatic drugs
- Bronchial asthma - Herbal medicine