People with bronchospasm find it hard to breathe, coughs, wheezes when breathing and complains of chest tightness. The presence of cough is linked to the increased production of mucus by the mucous membrane of occluded bronchi and bronchioles.
The main causes of bronchospasm are asthma and bronchitis; these two conditions are both inflammatory.
Often, physical examination and evaluation of the patient's medical history are sufficient for a definitive diagnosis.
The therapy is pharmacological and consists of medicines for opening the airways (beta2-agonists and anticholinergic bronchodilators) and anti-inflammatory drugs for reducing the inflammatory state (corticosteroids).
Anatomy of the bronchi and bronchioles
The bronchi represent the airways following the trachea.
In adults, the trachea bifurcates at the level of the 4th-5th thoracic vertebrae to give rise to the two primary (or main) bronchi, one for the right lung and one for the left lung.
The primary bronchi are in turn subdivided into ever lower caliber branches, constituting what in medical jargon is called the bronchial tree.
The bronchial tree consists of airways (or respiratory) external to the lungs (primary extrapulmonary bronchi) and intrapulmonary airways (secondary and tertiary bronchi, bronchioles, terminal bronchioles and respiratory bronchioles).
Similarly to the upper airways (which are: the nasal cavities, the nasopharynx, the pharynx, the larynx and the trachea), the bronchi have the function of transporting the air coming from the external environment to the functional units of the lungs: the so-called alveoli .
Surrounded by a dense network of capillaries, the alveoli are small sacs, which receive the inhaled air and allow the blood to "charge" with the oxygen necessary for the whole organism. It is in the alveoli, in fact, that the gaseous exchange of oxygen takes place. - carbon dioxide between the blood, circulating in the capillaries, and the atmospheric air, introduced by breathing.
From the histological point of view, the bronchi-bronchiole system tends to progressively change its structure as it penetrates more and more into the lungs: in the primary bronchi, the cartilage component is superior to the muscular one (there is a remarkable similarity with the trachea) ; starting from the secondary bronchi and until just before the alveoli, the muscular component takes over and gradually replaces the cartilage one.
of the bronchi or bronchioles, which causes a narrowing, or in particularly severe cases a "complete occlusion, of the airways.
Total narrowing or occlusion is usually temporary, so sooner or later there is a restoration of the patency of the airways.
MAIN CONSEQUENCES OF BRONCHOSPASM
An individual suffering from bronchospasm finds it difficult to breathe, as there is an impediment to the passage of air through the bronchi and / or bronchioles.
The situation, however, is slightly more complex than one might think. In fact, the narrowing or occlusion induces the bronchial mucosa to produce large quantities of mucus, which:
- helps to block the air entering the lungs,
- irritates the inner wall of the bronchi (or bronchioles) by inflaming it
- favors the onset of cough (N.B: cough is a defensive mechanism, which serves to expel this obstructive mucus).

Figure: Comparison between the respiratory airways of an asthmatic suffering from bronchospasm and a healthy individual. You can notice the narrowing of the passage for the air and the presence of mucus (in yellow). From the site: grosiramazing.com
Infectious agents that can cause bronchitis and, subsequently, episodes of bronchospasm.
- Influenza viruses
- Syncytial virus
- Adenovirus
- Haemophilus influenzae
- Streptococcus pneumoniae
- Moraxella catarrhalis
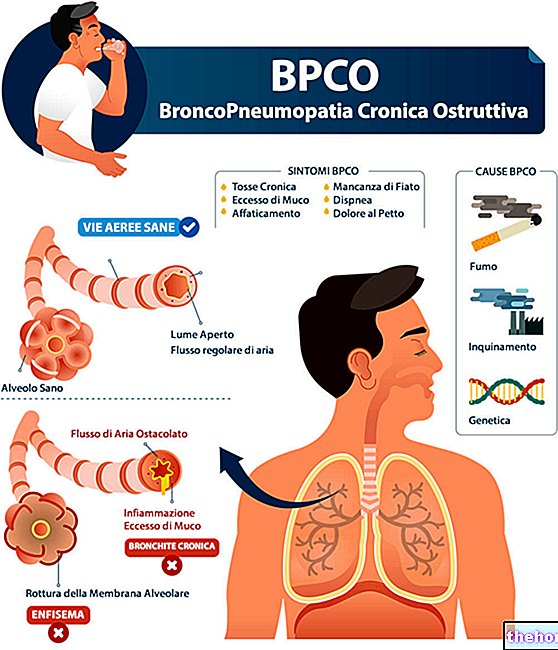
Bronchitis, on the other hand, can be an acute or chronic circumstance, which arises due to respiratory infections (such as colds or flu), cigarette smoke and / or pollution (environmental, domestic or work). Chronic forms of bronchitis represent a morbid state also known as chronic obstructive pulmonary disease (COPD).
* Allergens are substances that the body recognizes and interprets as foreign and potentially dangerous, therefore deserving of an immune attack aimed at their neutralization.
OTHER CAUSES
In apparently healthy individuals, bronchospasm episodes can also be caused by:
- Contact or proximity to particular substances (including pollen, dust, food, mold, animal hair, etc.), to which there is an "intolerance or" allergy.
- A physical activity that is intense or too high in relation to the possibilities of the individual who carries it out.
- The intake of certain drugs, including antibiotics, NSAIDs and antihypertensives. The possibility of causing bronchospasm is generally linked to a patient's intolerance towards the aforementioned drugs.
- General anesthesia, practiced in surgery, before certain very invasive operations. In these situations, bronchospasm represents a complication.
Its establishment is subsequent to the application, by the doctor, of the tube that is used to support the patient's breathing during the operation.
RISK FACTORS
All asthmatics, bronchitis sufferers, people exposed to bronchitis triggers (infectious diseases, polluted environments, etc.) and individuals allergic to some of the substances mentioned above are obviously at high risk of bronchospasm.
that characterize bronchospasm are:
- Cough. The mechanism that triggers the cough has already been addressed.
- Wheezing and wheezing. In people with asthma or chronic bronchitis, these breathing difficulties typically worsen in the evening, early morning, or after physical activity.
- Presence of rales when breathing. These are abnormal sounds that the patient emits during the breaths.
- Chest tightness. It is similar to a sense of pressure in the chest. Sometimes, it can feel like real pain.
COMPLICATIONS
If the bronchospasm is particularly severe and not properly treated, breathing difficulties may last long enough to cause the patient to die from asphyxiation.
The clinical manifestations that characterize the presence of severe breathing difficulties are: dyspnea at rest, cyanosis (usually in the fingers) and an increase in heart rate.

WHEN TO SEE THE DOCTOR?
According to doctors, it is good to contact them in the presence of:
- Cough that shows no signs of passing
- Rattles when breathing, which, instead of getting better, get worse
- Fever
- Minor breathing problems
Furthermore, always according to the opinion of the experts, these are symptoms that require an immediate medical examination:
- Cough with blood
- Dyspnea and cyanosis of the fingers
- Chest Pain
- The marked increase in heart rate
INSTRUMENTAL TESTS
The instrumental tests, which doctors use to reach a definitive diagnosis and investigate the triggering causes, are:
- Chest X-ray. It provides a "fairly clear picture of the lungs and other structures within the chest. Shows any signs of a" lung infection. It is a painless test, but still minimally invasive, as it exposes the patient to a (very low) dose of ionizing radiation.
- Spirometry. Fast, practical and painless, spirometry records the inspiratory and expiratory capacity of the lungs, and the patency (ie the opening) of the airways passing through the latter.
- CT scan (computerized axial tomography). It provides very comprehensive three-dimensional images of the organs contained in the thoracic cavity. It is therefore able to show most of the abnormalities that can affect the lungs (signs of infection, signs of inflammation, etc.).
It involves exposing the patient to a non-negligible dose of ionizing radiation, so it is to be considered an invasive test (albeit completely painless).
Under certain circumstances, to increase the quality of the images, the doctor administers a contrast agent into the patient's bloodstream. If used, this substance increases the invasiveness level of the examination, as it can trigger an allergic reaction (N.B: this generally occurs in predisposed subjects).
BETA2-AGONISTS
Beta2-agonists are norepinephrine derivatives.
These drugs are particularly suitable for relieving the symptoms that characterize acute asthma attacks, as they are able to release the smooth muscles of the bronchi and bronchioles in a very short time.
Effective even when the causes are not of an asthmatic nature, the most used beta2-agonists are:
- Salbutamol
- Salmeterol
- The formoterol
Please note: beta2-agonists do not reduce the inflammatory state of the bronchial tree; therefore their action is limited to the improvement of the symptomatological picture.
ANTICOLINERGIC BRONCHODILATORS
As you can guess from the name, anticholinergic bronchodilators dilate the respiratory tract, acting on the bronchial muscles. The ultimate purpose of their intake is to allow the patient to breathe better.
There are two categories of anticholinergic bronchodilators: short-acting anticholinergic bronchodilators and long-lasting anticholinergic bronchodilators. The former come into action in a very short time, which makes them particularly suitable for acute episodes of bronchospasm; the latter act with longer times, which makes them suitable medicines to prevent future episodes of bronchospasm.
The most commonly administered anticholinergic bronchodilators include ipratropium bromide and isoetarin.
Please note: like beta2-agonists, anticholinergic bronchodilators also relieve only the symptoms (they do not improve the inflammatory state that can affect bronchi and bronchioles).
INHALED (OR INHALED) CORTISTEROIDS
Belonging to the category of steroid drugs, inhaled corticosteroids reduce inflammation of the respiratory tract. Their use allows the patient to breathe better and relieve breathing difficulties.
Like all other steroid drugs, inhaled corticosteroids, when taken in excessive doses or for long periods of time, cause various side effects, some of which are very serious.
Possible side effects of steroid drugs.
- Hypertension
- Diabetes
- Weakening of the bones or osteoporosis
- Glaucoma
- Overweight or obesity
- Gastric ulcers
These are some of the most important preventive measures against the onset of bronchospasm.