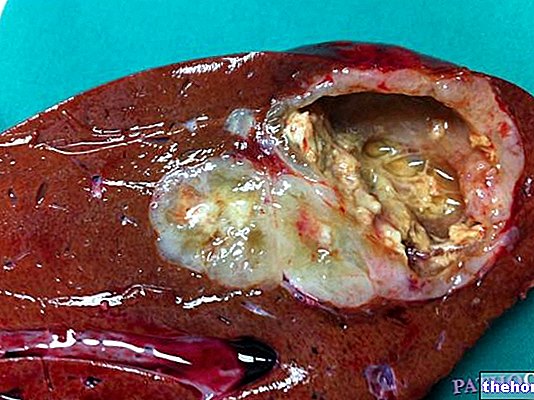
In this video we continue to talk about colorectal cancer. In the previous episode we saw what it consists of and why it arises. Today, we will understand how it can be recognized and what therapeutic choices are available. Briefly, before continuing, I will summarize some key points seen in the previous episode. Colorectal cancer arises in the terminal tract of the intestine due to an uncontrolled proliferation of some cells of the mucosa; this proliferation is due to a series of mutations that these cells accumulate over time, until they acquire characters of malignancy. It is not clear what exactly triggers this phenomenon, even if genetic predisposition and some dietary factors, such as the abuse of red meat and lack of fiber, undoubtedly play a favoring role. In any case, it is a slow process that generally passes through the formation of a polyp, which then with the slow passage of time becomes malignant; the polyps most at risk are the adenomatous ones. Thanks to this slow evolution, if diagnosed early, colorectal cancer can be treated with excellent chances of recovery.
Colorectal cancer tends not to show signs of itself for a long time. Furthermore, the first symptoms are often non-specific and can be confused, for example, for problems with hemorrhoids or anal fissures. In fact, the first alarm bell to pay attention to is the presence of traces of blood in the stool or on toilet paper, a characteristic sign of these much more common conditions. Sometimes, however, bleeding associated with colorectal cancer is not visible to the naked eye, so it can only be detected through a stool test. The test is known as the search for “occult blood in the stool” and while it is quite simple, it requires strict adherence to the procedures for collecting fecal samples. Another nonspecific signal that nevertheless deserves attention is the protracted change in intestinal habits, hence the sudden and prolonged onset of chronic constipation or diarrhea, or the alternation of the two disorders. Only when the tumor enters the most advanced stages, in relation to its location and extension, can abdominal pain, vomiting, abundant mucus discharge with the stool and tenesmus, or the continuous urge to defecate not accompanied by the emission of stools appear. then other symptoms appear, such as fatigue, anemia, lack of appetite, rapid weight loss and intestinal obstruction. Colorectal cancer can spread by direct extension to adjacent structures and metastasize by lymphatic or blood. The sites most often affected from metastatic spread are the liver, regional lymph nodes, lungs and bones.
In the face of suspicious symptoms, the diagnostic process begins with the "clinical examination of the patient. The doctor will perform a" rectal examination and palpate the abdomen to look for any masses in the intestine, liver and lymph nodes. I remember that it is precisely at the level of the rectum and the sigma that most of the colorectal tumors are located, while in the remaining tracts of the large intestine the neoplasms are less common. Useful information can also derive from blood tests, which in the presence of the tumor can show the "increase in tumor markers, such as CEA and CA 19.9. In any case, it is only with in-depth instrumental investigations that a certain diagnosis is reached." possible tumor staging. In addition to ascertaining its presence, these tests therefore allow to define its extension, aggressiveness, relations with surrounding organs, the state of the lymph nodes and any metastases present. Among these investigations, the most specific examination is colonoscopy, which, thanks to the possibility of performing a biopsy, allows for a histological analysis of the suspect tissue. I remind you briefly that colonoscopy allows visual exploration of the colon and rectum through a thin and flexible probe with a camera at its end. Furthermore, the examination has a very important additional advantage; in fact, it allows the polyps detected during the examination to be removed immediately with polypectomy. This eliminates the risk that these may evolve into a malignant tumor in the future. In addition to colonoscopy, further examinations can be performed, such as computed tomography (which we all know as CT) with contrast medium and ultrasound of the abdomen; these investigations are useful for establishing the degree of tumor infiltration in the bowel wall and the situation of the lymph nodes. To check for metastases, further investigations can be performed, such as a chest X-ray, liver ultrasound and bone scan. Sometimes magnetic resonance imaging or positron emission tomography (PET) imaging is also used for this purpose.
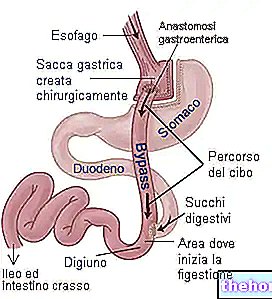
The treatment of colorectal cancers includes different types of interventions, to be chosen carefully based on the characteristics of the patient and the tumor. Currently, surgery is the form of treatment that offers the greatest guarantees. If the cancer is at a very early stage, only a small part of the intestinal tract affected by the disease can be removed. In severe cases, however, it is necessary to remove the entire intestinal tract involved and, sometimes, even the satellite lymph nodes. Generally, it is possible to rejoin the two remaining intestinal flaps and fully recover intestinal function. When this is not possible, it is necessary, instead, to resort to a temporary or permanent stoma; in these cases, the doctor creates an opening on the abdomen that allows you to collect the feces with special aids. In other words, an artificial anus is created.
In addition to surgery, radiotherapy can be used to treat colorectal cancer. This form of treatment can be practiced before surgery in order to reduce the volume and extension of the tumor mass, thus facilitating its surgical removal. In cases of advanced and inoperable cancer, on the other hand, radiotherapy allows you to control the symptoms and slow down the progression of the tumor. Similarly, chemotherapy also plays a role both in the preparation for surgery and in the treatment of advanced disease in the presence of metastases. Additionally, chemotherapy can be used after surgery to prevent post-surgical tumor recurrence and metastasis. As an alternative to chemotherapy, immunotherapy may be indicated, which involves the use of biological drugs capable of interacting with vital components of cancer cells, with the aim of slowing the evolution of the disease. However, biological therapies can only be used in particular cases. In general, the most important prognostic factor for colorectal cancer is the extent of the disease at the time of diagnosis.
There are some preventative interventions that can reduce the risk of developing colorectal cancer. First of all, we can intervene on diet and lifestyle. To prevent colorectal cancer, a low-fat diet is recommended, limited in the consumption of red meat and smoked, preserved and very salty foods. To protect us, however, we think of a balanced diet, rich in fiber, fruit and vegetables. The risk of colorectal cancer can also be reduced by practicing regular physical activity and correcting overweight. It is also reasonable to recommend that you stop smoking and drink alcohol in moderation. An effective prevention strategy consists in adhering to the screening campaign proposed by the National Health Service for all men and women from 50 years of age.Screening involves carrying out a test for the detection of occult blood in the faeces on the population at risk, on an annual or biennial basis; only in case of positivity, this will then be followed by colonoscopy. With these tests, it is often possible to intercept the disease in the early stages, therefore potentially treatable. However, the greatest impact prevention is the removal of precancerous lesions, such as polyps, which can precede tumor development by years. The early identification of these precursors and their endoscopic removal stops the progression towards malignancy and allows the disease to be prevented. Clearly, the individual program must be anticipated and agreed upon in high-risk subjects, especially in the presence of relatives with this tumor.




---sintomi-e-terapia.jpg)