Today we will talk about colorectal cancer, which in Italy represents the second most frequent neoplasm and also the second cause of death from cancer. In this first video we will see together what it is and what factors can favor its onset. In the next episode we will analyze instead the tests for the diagnosis and the possibilities of treatment.
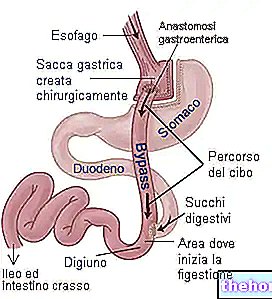
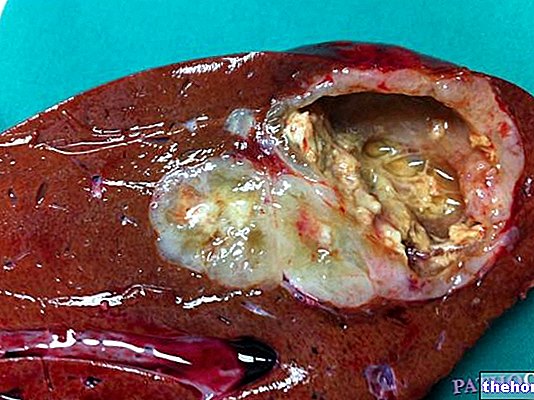
Colorectal cancer involves the last part of the intestine, called the large intestine or large intestine. I remind you briefly that the large intestine is the last section of the digestive system. Its appearance is that of a large tube, which starts from the cecum, continues in the colon, ends in the rectum and opens outwards through the anus. To be precise, large intestine and colon are therefore not exactly synonymous, since the colon is only a portion, albeit predominant, of the large intestine. The main function of the large intestine is to reabsorb mineral salts, water and vitamins produced by the local bacterial flora. Furthermore, it favors the progression of faeces and their accumulation in the rectal ampulla before being expelled to the outside. Colorectal cancer arises due to an uncontrolled proliferation of some cells that make up the mucous surface of the organ. We are therefore talking about the innermost lining of the intestinal wall, the one in direct contact with the faeces. part of the cases, this tumor originates from a pre-existing intestinal polyp The risk of a polyp degenerating into a tumor is generally low, but increases significantly for some types of polyps and for large polyps.
How to detect colorectal cancer Unfortunately, like many other cancers, that of the large intestine also tends not to show signs of itself for a long time. The alarm bells to pay attention to are blood loss with feces and persistent change in bowel habits; in practice, a medical check-up becomes advisable when a long period of inexplicable constipation arises or if periods of constipation and diarrhea alternate. To avoid unnecessary alarmism I remember that traces of blood in toilet paper are generally a sign of anal fissures or hemorrhoids, which are much more widespread and common disorders than colon cancer. Even changing bowel habits can recognize other root causes that have nothing to do with the cancer. However, it is good not to underestimate all these symptoms. When colorectal cancer enters an advanced stage, the symptoms become more specific. Abdominal pains of colic type, nausea and vomiting, evacuation of copious mucus with stool and tenesmus, or a continuous urge to evacuate, may occur. In addition, anemia, rapid weight loss or emission may occur. of hard and ribbon-like faeces, therefore very thin. Like other cancers, colorectal cancer can also give rise to metastases; it means that the disease can also extend to sites other than the colon due to the dissemination of neoplastic cells. Colorectal cancer metastases mostly occur in the liver, due to the connection of the two organs through the portal vein. Colorectal cancer affects men and women equally; according to the latest data provided by the Italian Cancer Registry Association, it occupies the third place for incidence in men, after prostate and lung cancer, and second place in women after breast cancer. In Italy, the figures are therefore impressive; roughly 38,000 new cases of colorectal cancer are diagnosed every year. Being often associated with aging, the increase in incidence recorded in recent years is largely explained by the generalized increase in the average age of population; in addition, an increase in sensitivity towards the problem should be emphasized with the execution of large generalized screening programs. Another very important fact is that in recent years there has been a decrease in mortality. An effective contribution, in this sense, is given above all by adequate information, preventive interventions and early diagnosis. Progress has also been made in the field of therapy: about 60% of patients diagnosed with colorectal cancer are in fact alive 5 years after diagnosis. Colorectal tumors, in fact, from the biological point of view, are generally neoplasms with a low malignant potential. The treatment, therefore, if applied early, is generally curative.
We anticipated that most colorectal cancers develop from the neoplastic transformation of pre-existing lesions, the so-called intestinal polyps. These are small protrusions of the mucosa, due to an altered cell proliferation, but initially benign. Among the different types of polyps, the most dangerous are the adenomatous ones, since, if left in place, they have a good chance of evolving into malignant forms within a short time. Screening tests, such as the search for traces of occult blood in the stool and colonoscopy, can help in the early identification of polyps, in order to remove them and thus prevent the formation of malignant tumors. It should be added that the so-called "adenoma-carcinoma sequence" is now known; these are all those phases that from a normal cell of the intestinal mucosa, passing through the formation of polyps, lead to the onset of the tumor. Without going into too much detail, the progression of the disease is due to the accumulation of a series of modifications at the gene level, which can be highlighted through specific diagnostic investigations. As for the actual causes, these are not yet fully clarified. There is probably no "single cause; rather, the tumor derives from" the interaction between genetic factors, written in our DNA, and specific environmental factors. We know, for example, that the chances of getting colorectal cancer increase in the presence of other pathological conditions, such as chronic inflammatory bowel diseases. People with ulcerative colitis or Crohn's disease, in fact, have a high risk of developing intestinal malignancy; in particular, this risk increases especially as the duration of the disease increases. As mentioned, it is possible to inherit the predisposition to get colorectal cancer from the parents; for this reason, if in the family of origin there are cases of pathologies due to specific genetic alterations, it is advisable to pay close attention and undergo regular screening tests. Among these pathologies, the familial adenomatous polyposis, Lynch syndrome and Gardner syndrome should be noted. Again in terms of genetic predisposition, it has been ascertained that the the probability of developing colorectal cancer increases if there are cases of first degree relatives - therefore parents, siblings or children - affected by this same neoplasm.
Turning to environmental factors, diet is believed to be the most important risk factor. Several scientific studies suggest, in particular, that a high-calorie diet, rich in animal fats and red meats, but low in fiber, may increase the risk of developing this cancer. On the contrary, a diet rich in fruit, vegetables and whole grains seems to play a protective role. However, it should be noted that incorrect eating habits are unlikely to be the only cause of colorectal cancer; certainly they can still contribute, in a negative sense, in the presence of other predisposing factors. These also include smoking, obesity, low physical activity and alcohol abuse. As with other cancers, the risk of getting sick increases with age. Although colorectal cancer can occur at any age, the disease is rare among young people and becomes more common from the age of 50 onwards. Starting from this age, in fact, prevention measures are generally recommended, such as the search for occult blood in the stool and colonoscopy. The first is recommended once a year or every two, while the second, certainly less appreciated but more reliable, can be repeated even once every 10 years.


---video.jpg)