Active ingredients: Bisoprolol (Bisoprolol fumarate)
Congescor 1.25 mg film-coated tablets
Congescor 2.5 mg film-coated tablets
Congescor 3.75 mg film-coated tablets
Congescor 5 mg film-coated tablets
Congescor 7.5 mg film-coated tablets
Congescor 10 mg film-coated tablets
Indications Why is Congescor used? What is it for?
The active ingredient contained in Congescor is bisoprolol. Bisoprolol belongs to the group of medicines called beta-blockers. These medicines work by affecting the body's response to certain nerve impulses, especially in the heart. As a result, bisoprolol slows the heart rate and makes the heart more efficient at pumping blood around the body.
Heart failure occurs when the heart muscle is weak and unable to pump enough blood to cover the body's needs. Congescor is used to treat stable chronic heart failure and is used in combination with other medicines available for this condition (such as ACE inhibitors, diuretics and cardiac glycosides).
Contraindications When Congescor should not be used
Do not take Congescor if you meet any of the following conditions:
- allergy (hypersensitivity) to bisoprolol or to any of the excipients (see section "What Congescor contains")
- severe asthma or severe chronic lung disease
- severe circulation problems in the extremities (such as Raynaud's syndrome), which can cause tingling or discolouration of the fingers (pale or blue) of the hands and feet
- untreated pheochromocytoma, a rare tumor of the adrenal gland
- metabolic acidosis, a condition characterized by too much acid in the blood.
Do not take Congescor if you have any of the following heart problems:
- acute heart failure
- worsening of heart failure requiring injection of medicines intravenously, which increases the force of contraction of the heart
- low heart rate
- low blood pressure
- certain heart conditions that cause a very slow heart rate or irregular heartbeat
- cardiogenic shock, a severe acute heart condition that causes low blood pressure and circulatory decompensation.
Precautions for use What you need to know before taking Congescor
If you have any of the following, tell your doctor before taking Congescor; your doctor may take special measures (for example by prescribing additional treatment or carrying out more frequent checks):
- diabetes
- tight fasting
- certain heart diseases, such as heart rhythm disturbances or severe chest pain at rest (Prinzmetal's angina)
- kidney or liver problems
- less severe circulatory problems in the extremities
- less severe asthma or chronic lung disease
- history of peeling skin rashes (psoriasis)
- tumor of the adrenal gland (pheochromocytoma)
- thyroid disorder.
Also, tell your doctor if you are to receive:
- desensitizing therapy (for example, to prevent hay fever), because Congescor can ease an allergic reaction or make it more severe
- an anesthesia (for example, for surgery), because CONGESCOR can influence the body's reaction to this situation.
Children and adolescents
Congescor is not recommended for use in children and adolescents
For those who carry out sporting activities: the use of the drug without therapeutic necessity constitutes doping and can in any case determine positive anti-doping tests.
Interactions Which drugs or foods can modify the effect of Congescor
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
Do not take the following medicines with Congescor without special instructions from your doctor:
- certain medicines used to treat irregular or abnormal heart beat (class I antiarrhythmic medicines, such as quinidine, disopyramide, lidocaine, phenytoin, flecainide, propafenone)
- certain medicines used in the treatment of high blood pressure, angina pectoris or irregular heartbeat (calcium channel blockers such as verapamil and diltiazem)
- certain medicines used in the treatment of arterial hypertension, such as clonidine, methyldopa, moxonidine, rilmenidine.
However, do not stop taking these medicines without first checking with your doctor.
Before taking Congescor together with the following medicines, consult your doctor, who may require more frequent checks of your condition:
- certain medicines used in the treatment of high blood pressure or angina pectoris (calcium channel blockers of the dihydropyridine type, such as felodipine and amlodipine)
- certain medicines used to treat irregular or abnormal heart beat (class III antiarrhythmic medicines, such as amiodarone)
- locally applied beta-blockers (such as eye drops containing timolol for the treatment of glaucoma)
- certain medicines used in the treatment, for example, of Alzheimer's disease or in the treatment of glaucoma (parasympathomimetics such as tacrine or carbachol) or medicines used to treat acute heart problems (sympathomimetics such as isoprenaline and dobutamine)
- antidiabetic medicines, including insulin
- anesthetic agents (for example during surgery)
- digitalis, used in the treatment of heart failure
- non-steroidal anti-inflammatory medicines (NSAIDs), used to treat arthritis, pain or inflammation (eg ibuprofen or diclofenac)
- any medicine that can lower blood pressure as a desired or undesirable effect, such as antihypertensives, certain medicines for depression (tricyclic antidepressants such as imipramine or amitriptyline), certain medicines used in the treatment of "epilepsy or during" anesthesia (barbiturates such as phenobarbital) o certain medicines used to treat mental disorders characterized by loss of contact with reality (phenothiazines such as levomepromazine)
- mefloquine, used in the prevention and treatment of malaria
- medicines for the treatment of depression called monoamine oxidase inhibitors (except MAO-B inhibitors), such as moclobemide.
Warnings It is important to know that:
Pregnancy and breastfeeding
There is a risk that the use of CONGESCOR during pregnancy will harm the unborn child. If you are pregnant or wish to become pregnant, consult your doctor, who will decide whether you can take CONGESCOR if you are pregnant.
It is not known whether bisoprolol passes into breast milk. Therefore, it is recommended not to breastfeed while on Congescor therapy.
Driving and using machines
Your ability to drive and use machines may be affected depending on how well the medicine is tolerated. Use particular caution at the start of treatment, when the dose is increased, when switching from another medicine and in combination with alcohol.
Dose, Method and Time of Administration How to use Congescor: Posology
Always take this medicine exactly as your doctor has told you. If in doubt, consult your doctor or pharmacist.
Treatment with Congescor requires periodic monitoring by the physician. This is particularly necessary at the start of treatment, during dose escalation and upon discontinuation of treatment.
Take the tablets with some water in the morning, regardless of food. Do not crush or chew the tablet. The scored tablets can be divided into two equal doses
Treatment with Congescor is usually conducted over the long term.
Adults, including the elderly:
Treatment with bisoprolol is started in low doses, which are gradually increased. Your doctor will decide how to increase the dose, usually as follows:
- 1.25 mg bisoprolol once daily for one week
- 2.5 mg bisoprolol once daily for one week
- 3.75 mg bisoprolol once daily for one week
- 5 mg bisoprolol once daily for four weeks
- 7.5 mg bisoprolol once daily for four weeks
- 10 mg bisoprolol once daily for maintenance (long-term) therapy
The maximum recommended daily dose is 10 mg bisoprolol. Depending on how well the medicine is tolerated, your doctor may decide to extend the interval between dose increases. If your condition gets worse or you no longer tolerate the medicine, it may be necessary to reduce the dose again or stop treatment. In some patients a maintenance dose of less than 10 mg bisoprolol may be sufficient, your doctor will tell you what to do.
If you have to stop treatment completely, your doctor will probably advise you to reduce the dose gradually, otherwise your condition may get worse.
Overdose What to do if you have taken too much Congescor
If you take more Congescor than you should
If you have taken more Congescor tablets than you should, tell your doctor immediately, who will decide what steps are necessary. Symptoms of an overdose may include slow heart rate, severe breathing difficulties, dizziness and tremors (due to low blood sugar).
If you forget to take Congescor
Do not take a double dose to make up for a forgotten dose. Take your usual dose the next morning.
If you stop taking Congescor
Never stop taking Congescor without first checking with your doctor - your condition may get worse. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Side Effects What are the side effects of Congescor
Like all medicines, this medicine can cause side effects, although not everybody gets them. To prevent serious reactions, see your doctor immediately if a side effect is severe, comes on suddenly or gets worse quickly.
The most serious side effects are related to heart function:
- slow heart rate (affects more than 1 in 10 people)
- worsening of heart failure (affects less than 1 in 10 people)
- slow or irregular heartbeat (affects less than 1 in 100 people) If you feel dizzy, faint or have trouble breathing, see your doctor as soon as possible.
Other side effects are listed below, depending on how often they occur:
Common (affects less than 1 in 10 people):
- tiredness, feeling of weakness, dizziness, headache
- feeling cold or numb in the hands or feet
- low blood pressure
- stomach or intestinal problems such as nausea, vomiting, diarrhea or constipation.
Uncommon (affects less than 1 in 100 people):
- sleep disorders
- depression
- dizziness when standing up
- breathing problems in patients with asthma or chronic lung disease
- muscle weakness, muscle cramps.
Rare (affects less than 1 in 1,000 people):
- hearing problems
- allergic rhinorrhea
- reduced tear flow
- inflammatory process of the liver which can cause yellowing of the skin or the sclera of the eye
- results of certain blood tests for liver function or fat levels that differ from normal
- allergic-like reactions such as itching, flushing, skin rashes
- difficulty with erection
- nightmares, hallucinations.
- fainting
Very rare (affects less than 1 in 10,000 people):
- irritation and redness of the eyes (conjunctivitis)
- hair loss
- appearance or worsening of a peeling skin rash (psoriasis); psoriatic-like rash.
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
Expiry and Retention
- Keep this medicine out of the sight and reach of children
- Do not use this medicine after the expiry date which is stated on the blister and carton after "EXP". The expiry date refers to the last day of the month.
Congescor 1.25 mg film-coated tablets:
Congescor 2.5 mg film-coated tablets:
Congescor 3.75 mg film-coated tablets:
- Do not store above 25 ° C.
Congescor 5 mg film-coated tablets:
Congescor 7.5 mg film-coated tablets:
Congescor 10 mg film-coated tablets:
- Do not store above 30 ° C.
Do not throw any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. This will help protect the environment.
Box contents and other information
What it contains
Congescor Congescor 1.25 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 1.25 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; pregelatinised maize starch; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous).
Film coating: dimethicone; talc; macrogol 400; titanium dioxide (E171); hypromellose.
Congescor 2.5 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 2.5 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous).
Film coating: dimethicone; macrogol 400; titanium dioxide (E171); hypromellose.
Congescor 3.75 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 3.75 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous).
Film coating: yellow iron oxide (E172); dimethicone; macrogol 400; titanium dioxide (E171); hypromellose.
Congescor 5 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 5 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous).
Film coating: yellow iron oxide (E172); dimethicone; macrogol 400; titanium dioxide (E171); hypromellose.
Congescor 7.5 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 7.5 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous). Film coating: yellow iron oxide (E172); dimethicone; macrogol 400; titanium dioxide (E171); hypromellose.
Congescor 10 mg film-coated tablets
- The active ingredient is bisoprolol fumarate. Each film-coated tablet contains 10 mg.
- The excipients are:
Tablet core: anhydrous colloidal silica; magnesium stearate; crospovidone; cornstarch; microcrystalline cellulose; calcium hydrogen phosphate (anhydrous).
Film coating: red iron oxide (E172); yellow iron oxide (E172); dimethicone; macrogol 400; titanium dioxide (E171); hypromellose.
Description of what Congescor looks like and contents of the pack
Congescor 1.25 mg film-coated tablets are white and round.
Congescor 2.5 mg film-coated tablets are white and heart-shaped with a breakline on both sides.
Congescor 3.75 mg film-coated tablets are creamy white and heart-shaped with a breakline on both sides.
Cardicor 5 mg film-coated tablets are pale yellow and heart-shaped with a breakline on both sides.
Congescor 7.5 mg film-coated tablets are pale yellow and heart-shaped with a breakline on both sides.
Cardicor 10 mg film-coated tablets are pale to light orange and heart-shaped with a breakline on both sides.
Each pack contains 10, 20, 28, 30, 50, 56, 60, 90, or 100 tablets.
Not all pack sizes may be marketed.
Source Package Leaflet: AIFA (Italian Medicines Agency). Content published in January 2016. The information present may not be up-to-date.
To have access to the most up-to-date version, it is advisable to access the AIFA (Italian Medicines Agency) website. Disclaimer and useful information.
01.0 NAME OF THE MEDICINAL PRODUCT
CONGESCOR
02.0 QUALITATIVE AND QUANTITATIVE COMPOSITION
Congescor 1.25 mg
Each tablet contains 1.25 mg bisoprolol fumarate
Congescor 2.5 mg
Each tablet contains 2.5 mg of bisoprolol fumarate
Congescor 3.75 mg
Each tablet contains 3.75 mg of bisoprolol fumarate
Congescor 5 mg
Each tablet contains 5 mg of bisoprolol fumarate
Congescor 7.5 mg
Each tablet contains 7.5 mg of bisoprolol fumarate
Congescor 10 mg
Each tablet contains 10 mg of bisoprolol fumarate
For the full list of excipients, see section 6.1
03.0 PHARMACEUTICAL FORM
Film-coated tablets:
The scored tablets can be divided into two equal doses
04.0 CLINICAL INFORMATION
04.1 Therapeutic indications
Treatment of chronic, stable heart failure with reduced left ventricular function, in addition to ACE inhibitors and diuretics and possibly cardioactive glycosides (for further information see Section 5.1).
04.2 Posology and method of administration
Standard treatment of chronic heart failure consists of an ACE inhibitor (or an angiotensin receptor antagonist in case of intolerance to ACE inhibitors), a beta blocker, diuretics and, if appropriate, cardiac glycosides. At the start of treatment with bisoprolol, patients must be in stable clinical condition (without acute decompensation).
It is recommended that the physician has clinical experience in the treatment of chronic heart failure.
During the titration phase and thereafter, transient worsening of heart failure, hypotension and bradycardia may occur.
Dosage
Titration phase
Stable chronic heart failure therapy with bisoprolol requires a titration phase
Treatment with bisoprolol should be initiated with a gradual dose increase according to the following schedule:
• 1.25 mg once daily for 1 week, if well tolerated increase to
• 2.5 mg once daily for the following week, if well tolerated increase to
• 3.75 mg once daily for the following week, if well tolerated increase to
• 5 mg once daily for the following 4 weeks, if well tolerated increase to
• 7.5 mg once daily for the following 4 weeks, if well tolerated increase to
• 10 mg once daily for maintenance therapy.
The maximum recommended dose is 10 mg once a day.
During the titration phase, close monitoring of vital signs (heart rate, blood pressure) and symptoms of worsening heart failure is recommended.
Symptoms may already begin on the first day of treatment.
Modifications of the treatment
If the maximum recommended dose is not well tolerated, gradual dose reduction may be considered.
In the event of transient worsening of heart failure, hypotension or bradycardia, it is recommended that the dosage of concomitant therapy be re-examined. It may also be necessary to temporarily reduce the dose of bisoprolol or consider discontinuation.
Reintroduction and / or gradual dose escalation of bisoprolol should always be considered when the patient regains stability.
If discontinuation is decided, tapering of the dose is recommended, as abrupt withdrawal may lead to acute deterioration of the patient's condition.
Treatment of chronic, stable heart failure with bisoprolol is generally a long-term treatment.
Impaired renal or hepatic function
There is no information regarding the pharmacokinetics of bisoprolol in patients with chronic heart failure and impaired hepatic or renal function.
Dosage increases in these patients should be made with greater caution.
Senior citizens
No dose adjustments are required.
Pediatric population
There is no pediatric experience with bisoprolol, therefore its use is not recommended in pediatric patients.
Method of administration
Bisoprolol tablets should be taken in the morning and can be taken with food. They must be swallowed with liquid and not chewed.
04.3 Contraindications
Bisoprolol is contraindicated in patients with chronic heart failure in the presence of:
• acute heart failure or episodes of decompensated heart failure requiring intravenous inotropic therapy;
• cardiogenic shock;
• second or third degree atrioventricular block;
• sick sinus syndrome;
• sino-atrial block;
• symptomatic bradycardia;
• symptomatic hypotension;
• severe bronchial asthma or severe obstructive and chronic lung disease;
• severe form of peripheral arterial occlusion and Raynaud's syndrome;
• untreated pheochromocytoma (see Section 4.4);
• metabolic acidosis;
• hypersensitivity to bisoprolol or to any of the excipients listed in Section 6.1.
04.4 Special warnings and appropriate precautions for use
Treatment of stable chronic heart failure with bisoprolol should be initiated with a special titration phase.
Discontinuation of bisoprolol therapy, especially in patients with ischemic heart disease, should not be done abruptly unless necessary, as this may transiently aggravate the heart condition.
The initiation and cessation of bisoprolol treatment requires regular monitoring.
There is no therapeutic experience with bisoprolol in heart failure in patients with the following diseases and conditions:
• insulin dependent diabetes mellitus (type I);
• severe impairment of renal function;
• severe impairment of liver function;
• restrictive cardiomyopathy;
• congenital heart disease;
• hemodynamically significant organic valve diseases;
• myocardial infarction (within the previous 3 months).
Bisoprolol should be used with caution in case of:
• bronchospasm (bronchial asthma, obstructive airway diseases);
• diabetes mellitus with unstable blood sugar; symptoms of hypoglycemia can be masked
• strict fasting;
• ongoing desensitizing therapy. As with other beta-blockers, bisoprolol can increase both sensitivity to allergens and the severity of anaphylactic reactions. Treatment with adrenaline does not always produce the expected therapeutic effect;
• 1st degree atrioventricular block;
• Prinzmetal's angina;
• peripheral arterial occlusion (worsening of symptoms may occur especially at the start of therapy)
• general anesthesia
In patients undergoing general anesthesia, beta-blockade reduces the incidence of arrhythmias and myocardial ischaemia during induction and intubation, and in the postoperative period. It is currently recommended that any maintenance beta-blocker treatment be continued in the peri-operative period. The anesthetist should be advised of the use of the beta blocker due to potential interactions with other drugs which may cause bradyarrhythmias, alleviation of reflex tachycardia and decreased ability to reflexively compensate for blood loss.
If it is deemed necessary to discontinue beta-blocker therapy prior to surgery, discontinuation should be done gradually and completed approximately 48 hours prior to anesthesia.
The combination of bisoprolol with calcium channel blockers of the verapamil or diltiazem type, with class I antiarrhythmic drugs and centrally acting antihypertensive drugs, is generally not recommended; for details refer to paragraph 4.5.
In bronchial asthma or other chronic obstructive pulmonary diseases that can cause symptoms, concomitant therapy with bronchodilators should be given.
In individual cases, in patients with asthma, an increase in airway resistance may occur, therefore an increase in the dose of beta 2 stimulants may be necessary.
In patients with psoriasis or family history of psoriasis, the benefit-risk balance should be carefully evaluated before administration of beta-blockers (bisoprolol).
In patients with pheochromocytoma bisoprolol should not be administered separately by an alpha blocker.
Symptoms of thyrotoxicosis may be masked during bisoprolol therapy.
04.5 Interactions with other medicinal products and other forms of interaction
Combinations not recommended
Calcium channel blockers of the verapamil type and to a lesser extent of the diltiazem type: negative influence on contractility and atrio-ventricular conduction.
Intravenous administration of verapamil in patients on beta-blocker treatment may lead to marked hypotension and atrioventricular block.
Class I antiarrhythmic drugs (eg quinidine, disopyramide, lidocaine, phenytoin; flecainide, propafenone): the effect on atrioventricular conduction time can be potentiated and the negative inotropic effect can be increased.
Centrally acting antihypertensive drugs such as clonidine and others (eg methyldopa, moxonidine, rilmenidine): Concomitant use of centrally acting antihypertensive drugs may worsen heart failure by a decrease in central sympathetic tone (reduction in heart rate and output , vasodilation). Abrupt discontinuation, particularly if prior to discontinuation of the beta blocker, may increase the risk of "rebound hypertension".
Combinations to be used with caution
Dihydropyridine calcium channel blockers, such as felodipine and amlodipine: Concomitant use may increase the risk of hypotension and the risk of further deterioration of the functional status of the ventricular pump in patients with heart failure cannot be excluded.
Class III antiarrhythmic drugs (eg amiodarone): the effect on atrio-ventricular conduction time can be potentiated.
Topical beta-blockers (e.g. eye drops for the treatment of glaucoma) may have an additive effect to the systemic effects of bisoprolol.
Parasympathomimetic Drugs: Concomitant use may increase atrioventricular conduction time and the risk of bradycardia.
Insulin and oral antidiabetics: increased hypoglycaemic effect. Blockade of beta receptors may mask the onset of hypoglycaemic symptoms.
Anesthetic agents: Attenuation of reflex tachycardia and increased risk of hypotension (for more information on general anesthesia see also section 4.4).
Digitalis glycosides: reduced heart rate, increased atrio-ventricular conduction time.
Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs may reduce the hypotensive effect of bisoprolol.
Beta agents-sympathomimetics (such as isoprenaline, dobutamine): the combination with bisoprolol can reduce the effect of these drugs.
Sympathomimetics that activate both beta- and alpha-adrenoceptors (such as norepinephrine, adrenaline): combination with bisoprolol may unmask the vasoconstrictive effects of these alpha-mediated agents, leading to increased blood pressure and worsening of claudication intermittent. Such interactions are considered more likely with non-selective beta-blockers.
Concomitant use of antihypertensive agents as well as other drugs with a potential blood pressure lowering effect (such as tricyclic antidepressants, barbiturates, phenothiazines) may increase the risk of hypotension.
Associations to keep in mind
Mefloquine: increased risk of bradycardia.
Monoamine oxidase inhibitors (except MAO B inhibitors): increased hypotensive effect of beta-blockers but also risk of hypertensive crisis.
04.6 Pregnancy and lactation
Pregnancy
Bisoprolol has pharmacological effects which may lead to harmful effects during pregnancy and / or in the fetus / newborn. In general, beta-blockers reduce placental perfusion, which is associated with fetal growth retardation, intrauterine death, abortion or premature birth. Undesirable effects (e.g. hypoglycaemia and bradycardia) may occur in the fetus and neonate. If beta-blocker therapy is required, selective beta-1 blockers are preferred. Bisoprolol should not be used during pregnancy unless clearly necessary. In this case, monitor the utero-placental blood flow and fetal growth. Consider alternative therapies in case of harmful effects on pregnancy and the fetus. Monitor the neonate closely as symptoms of hypoglycemia and bradycardia usually occur within the first three days.
Feeding time
It is not known whether the drug is excreted in human milk. Therefore it is not recommended to take bisoprolol while breastfeeding.
04.7 Effects on ability to drive and use machines
In a clinical study, in patients with coronary artery disease, bisoprolol was found not to adversely affect the ability to drive. However, due to individual variations in drug reactions, the ability to drive and use machines may be affected. This must be considered in particular at the start of therapy, in the event of a change in therapy and in the case of simultaneous alcohol intake.
04.8 Undesirable effects
The following definitions are used to indicate the frequency of undesirable effects:
Cardiac pathologies
Very common: bradycardia.
Common: worsening of heart failure.
Uncommon: AV conduction disturbances.
Diagnostic tests
Rare: increased triglycerides, increased liver enzymes (ALAT, ASAT).
Nervous system disorders
Common: dizziness, headache.
Rare: syncope.
Eye disorders
Rare: reduced lacrimation (to be taken into account in the case of use of contact lenses).
Very rare: conjunctivitis.
Ear and labyrinth disorders
Rare: hearing disorders.
Respiratory, thoracic and mediastinal disorders
Uncommon: bronchospasm in patients with bronchial asthma or a history of obstructive respiratory disease.
Rare: allergic rhinitis.
Gastrointestinal disorders
Common: gastrointestinal disturbances such as nausea, vomiting, diarrhea, constipation.
Skin and subcutaneous tissue disorders
Rare: hypersensitivity reactions (itching, redness, rash).
Very rare: alopecia. Beta blockers can cause or worsen psoriasis or induce pseudo-psoriatic rashes.
Musculoskeletal and connective tissue disorders
Uncommon: muscle weakness and cramps.
Vascular pathologies
Common: feeling of coldness or tingling in the extremities, hypotension.
Uncommon: orthostatic hypotension.
Systemic pathologies
Common: asthenia, fatigue.
Hepatobiliary disorders
Rare: hepatitis.
Diseases of the reproductive system and breast
Rare: disorders of male sexual function.
Psychiatric disorders
Uncommon: sleep disturbances, depression.
Rare: nightmares, hallucinations.
04.9 Overdose
Following overdose (e.g. a daily dose of 15 mg instead of 7.5 mg), third degree A-V block, bradycardia, and dizziness have been reported. In general, the most common symptoms expected in the event of an overdose are: bradycardia, hypotension, bronchospasm, acute heart failure and hypoglycemia. Few cases of overdose with bisoprolol (maximum dose: 2000 mg) have been reported to date in patients with hypertension and / or coronary artery disease who have experienced bradycardia and / or hypotension; all patients recovered. There is "a" large individual variability in sensitivity to a single high dose of bisoprolol and heart failure patients are likely to be very sensitive. It is therefore mandatory to start the therapy of these patients with a gradual titration according to the scheme reported in par. 4.2.
In the event of overdose, bisoprolol treatment should be discontinued and supportive and symptomatic therapy instituted. Limited data suggest that bisoprolol is difficult to dialyzable. Based on the expected pharmacological actions and recommendations of other beta-blockers, the following general measures should be considered when clinically justified.
Bradycardia: administer intravenous atropine. If the response is inadequate, isoprenaline or another drug with positive chronotropic properties may be administered with caution. In some circumstances it may be necessary to insert a transvenous pacemaker.
Hypotension: Intravenous fluids and vasopressors should be administered. Intravenous administration of glucagon may be helpful.
Atrioventricular block (degree II or III): Patients should be monitored closely and treated with isoprenaline infusion or a transvenous pacemaker may need to be introduced.
Acute worsening of heart failure: administer intravenous diuretics, inotropic drugs, vasodilators.
Bronchospasm: Administer bronchodilators such as isoprenaline, beta-2 sympathomimetic drugs and / or aminophylline.
Hypoglycemia: administer intravenous glucose.
05.0 PHARMACOLOGICAL PROPERTIES
05.1 Pharmacodynamic properties
Pharmacotherapeutic group: b-blocking agents, selective, ATC code: C07AB07
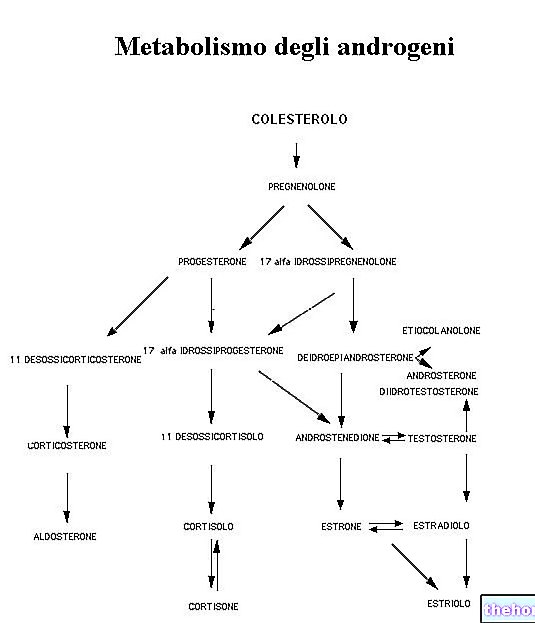
Bisoprolol is a highly selective beta-blocker for beta-1 receptors, devoid of intrinsic sympathomimetic activity (ISA) and related membrane stabilizing activity. It has a low affinity for beta-2 receptors of bronchial and vascular smooth muscle as well as for beta-2 receptors that regulate metabolism. Consequently, bisoprolol is generally not expected to affect airway resistance and beta-2 receptor mediated metabolic effects.
The selectivity of bisoprolol towards beta-1 receptors is not dose dependent.
A total of 2647 patients were included in the CIBIS II clinical trial.
83% (n = 2202 patients) were NYHA class III patients, while 17% (n = 445 patients) were NYHA class IV. Patients had stable, symptomatic heart failure (ejection fraction ≤ 35 %, detected on echocardiography). Total mortality decreased from 17.3% to 11.8% (relative reduction of 34%).
In addition, a reduction in sudden deaths (3.6% vs 6.3%, with a relative reduction of 44%) and a reduced number of heart failure episodes requiring hospitalization (12% vs 17.6%, relative reduction of 36%).
Finally, a significant improvement in functional status was shown in patients (NYHA class). During the initial and titration phase of bisoprolol there were hospitalizations due to bradycardia (0.53%), hypotension (0.23%) and acute decompensation (4.97%), but in a similar percentage to the placebo group (0 %, 0.3% and 6.74%).
During the entire study period the number of strokes fatal and disabling was 20 in the bisoprolol group and 15 in the placebo group.
The CIBIS III study examined 1,010 patients ≥ 65 years of age with mild or moderate chronic heart failure (CHF; NYHA class II or III) and left ventricular ejection fraction ≥ 35% who were not previously treated with ACE inhibitors, beta blockers or angiotensin receptor antagonists.
After an initial 6-month treatment period with bisoprolol or enalapril, patients were treated with a combination of bisoprolol and enalapril for a period of 6 to 24 months.
There was a trend towards a higher rate of worsening of chronic heart failure when bisoprolol was administered in the first 6 months of treatment.
Non-inferiority of initial treatment with bisoprolol compared to initial treatment with enalapril was not demonstrated in the "per-protocol" analysis, although the two treatment initiation strategies for chronic heart failure showed a similar frequency of the end point. primary combined death and hospitalization at the end of the study (32.4% in the group initially treated with bisoprolol vs. 33.1% in the group initially treated with enalapril; per-protocol population).
The study shows that bisoprolol can also be used in elderly patients with mild or moderate chronic heart failure.
Bisoprolol is also used for the treatment of hypertension and angina.
Acute administration of bisoprolol in patients with coronary artery disease without chronic heart failure reduces heart rate, systolic output and consequently cardiac output and oxygen consumption. In chronic administration the high initial peripheral resistance decreases.
05.2 Pharmacokinetic properties
Absorption
The absorption and bioavailability of bisoprolol after oral administration reaches 90%.
Distribution
The volume of distribution is 3.5 l / kg. The plasma protein binding of bisoprolol is approximately 30%.
Biotransformation and elimination
Bisoprolol is eliminated from the body by two routes: about 50% is transformed into inactive metabolites in the liver, then eliminated by the kidney; while the remaining 50% is excreted unchanged via the kidney. Total clearance is about 15 l / h. The plasma half-life of 10-12 hours allows 24 hours of therapeutic efficacy after once daily administration.
Linearity
The kinetics of bisoprolol are linear and independent of age.
Special populations
Since excretion occurs equally in the kidney and liver, no dosage adjustment is normally required in patients with hepatic impairment or renal insufficiency.
Pharmacokinetic parameters in patients with chronic, stable heart failure and with impaired hepatic or renal function have not yet been studied.
Plasma levels and half-life of bisoprolol in patients with chronic, stable heart failure (NYHA class III) are prolonged compared to healthy volunteers.
The maximum plasma concentration at the steady state is 64 ± 21 ng / ml for a daily dose of 10 mg and the half-life is 17 ± 5 hours.
05.3 Preclinical safety data
Non-clinical data reveal no particular risk for humans based on studies on safety, repeated dose toxicity, genotoxicity and carcinogenic potential.
Like other beta-blockers bisoprolol caused pregnancy toxicity (decreased food intake or weight loss) and embryo-fetal toxicity (increased incidence of resorption, decreased birth weight and delayed physical development) at high doses. but it showed no teratogenic effects.
06.0 PHARMACEUTICAL INFORMATION
06.1 Excipients
Congescor 1.25 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, pregelatinised maize starch, maize starch, microcrystalline cellulose, anhydrous calcium hydrogen phosphate.
Coating film: dimethicone, talc, macrogol 400, titanium dioxide (E 171), hypromellose.
Congescor 2.5 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, microcrystalline cellulose, corn starch, anhydrous calcium hydrogen phosphate.
Coating film: dimethicone, macrogol 400, titanium dioxide (E 171), hypromellose.
Congescor 3.75 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, microcrystalline cellulose, corn starch, anhydrous calcium hydrogen phosphate.
Coating film: yellow iron oxide (E 172), dimethicone, macrogol 400, titanium dioxide (E 171), hypromellose.
Congescor 5 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, microcrystalline cellulose, corn starch, anhydrous calcium hydrogen phosphate.
Coating film: yellow iron oxide (E 172), dimethicone, macrogol 400, titanium dioxide (E 171), hypromellose.
Congescor 7.5 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, microcrystalline cellulose, corn starch, anhydrous calcium hydrogen phosphate.
Coating film: yellow iron oxide (E 172), dimethicone, macrogol 400, titanium dioxide (E 171), hypromellose.
Congescor 10 mg
Tablet: anhydrous colloidal silica, magnesium stearate, crospovidone, microcrystalline cellulose, corn starch, anhydrous calcium hydrogen phosphate.
Coating film: red iron oxide (E 172), yellow iron oxide (E 172), dimethicone, macrogol 400, titanium dioxide (E 171), hypromellose.
06.2 Incompatibility
Not relevant.
06.3 Period of validity
Congescor 1.25 mg, 2.5 mg and 3.75 mg: 3 years.
Congescor 5 mg, 7.5 mg and 10 mg: 5 years.
06.4 Special precautions for storage
Congescor 1.25 mg, 2.5 mg and 3.75 mg: do not store above 25 ° C.
Congescor 5 mg, 7.5 mg and 10 mg: do not store above 30 ° C.
06.5 Nature of the immediate packaging and contents of the package
The container is a blister consisting of a polyvinyl chloride film and covered with an aluminum foil.
Cartons of: 10, 20, 28, 30, 50, 56, 60, 90 and 100 tablets.
Not all pack sizes may be marketed
06.6 Instructions for use and handling
No special instructions.
07.0 MARKETING AUTHORIZATION HOLDER
Daiichi Sankyo Italia SpA via Paolo di Dono 73, Rome
08.0 MARKETING AUTHORIZATION NUMBER
Congescor 20 tablets of 1.25 mg - AIC n. 034953012 / M
Congescor 28 tablets of 1.25 mg - AIC n. 034953024 / M
Congescor 30 tablets of 1.25 mg - AIC n. 034953036 / M
Congescor 50 tablets of 1.25 mg - AIC n. 034953048 / M
Congescor 56 tablets of 1.25 mg - AIC n. 034953051 / M
Congescor 60 tablets of 1.25 mg - AIC n. 034953063 / M
Congescor 90 tablets of 1.25 mg - AIC n. 034953075 / M
Congescor 100 tablets of 1.25 mg - AIC n. 034953481 / M
Congescor 20 tablets of 2.5 mg - AIC n. 034953087 / M
Congescor 28 tablets of 2.5 mg - AIC n. 034953099 / M
Congescor 30 tablets of 2.5 mg - AIC n. 034953101 / M
Congescor 50 tablets of 2.5 mg - AIC n. 034953113 / M
Congescor 56 tablets of 2.5 mg - AIC n. 034953125 / M
Congescor 60 tablets of 2.5 mg - AIC n. 034953137 / M
Congescor 90 tablets of 2.5 mg - AIC n. 034953149 / M
Congescor 100 tablets of 2.5 mg - AIC n. 034953152 / M
Congescor 20 tablets of 3.75 mg - AIC n. 034953164 / M
Congescor 28 tablets of 3.75 mg - AIC n. 034953176 / M
Congescor 30 tablets of 3.75 mg - AIC n. 034953188 / M
Congescor 50 tablets of 3.75 mg - AIC n. 034953190 / M
Congescor 56 tablets of 3.75 mg - AIC n. 034953202 / M
Congescor 60 tablets of 3.75 mg - AIC n. 034953214 / M
Congescor 90 tablets of 3.75 mg - AIC n. 034953226 / M
Congescor 100 tablets of 3.75 mg - AIC n. 034953238 / M
Congescor 20 tablets of 5 mg - AIC n. 034953240 / M
Congescor 28 tablets of 5 mg - AIC n. 034953253 / M
Congescor 30 tablets of 5 mg - AIC n. 034953265 / M
Congescor 50 tablets of 5 mg - AIC n. 034953277 / M
Congescor 56 tablets of 5 mg - AIC n. 034953289 / M
Congescor 60 tablets of 5 mg - AIC n. 034953291 / M
Congescor 90 tablets of 5 mg - AIC n. 034953303 / M
Congescor 100 tablets of 5 mg - AIC n. 034953315 / M
Congescor 20 tablets of 7.5 mg - AIC n. 034953327 / M
Congescor 28 tablets of 7.5 mg - AIC n. 034953339 / M
Congescor 30 tablets of 7.5 mg - AIC n. 034953341 / M
Congescor 50 tablets of 7.5 mg - AIC n. 034953354 / M
Congescor 56 tablets of 7.5 mg - AIC n. 034953366 / M
Congescor 60 tablets of 7.5 mg - AIC n. 034953378 / M
Congescor 90 tablets of 7.5 mg - AIC n. 034953380 / M
Congescor 100 tablets of 7.5 mg - AIC n. 034953392 / M
Congescor 20 tablets of 10 mg - AIC n. 034953404 / M
Congescor 28 tablets of 10 mg - AIC n. 034953416 / M
Congescor 30 tablets of 10 mg - AIC n. 034953428 / M
Congescor 50 tablets of 10 mg - AIC n. 034953430 / M
Congescor 56 tablets of 10 mg - AIC n. 034953442 / M
Congescor 60 tablets of 10 mg - AIC n. 034953455 / M
Congescor 90 tablets of 10 mg - AIC n. 034953467 / M
Congescor 100 tablets of 10 mg - AIC n. 034953479 / M
09.0 DATE OF FIRST AUTHORIZATION OR RENEWAL OF THE AUTHORIZATION
Date of first authorization: 5 April 2002
Date of last renewal: June 2009
10.0 DATE OF REVISION OF THE TEXT
October 2012


















-nelle-carni-di-maiale.jpg)