Generality
Urobilin is a substance derived from the reduction of bilirubin by the intestinal bacterial flora.

A small amount of urobilin is instead reabsorbed and conveyed to the liver, then excreted again in the intestine through the bile.
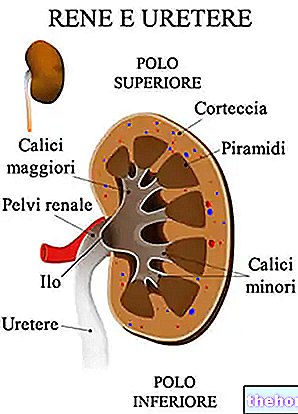
Particularly modest, in normal conditions, is the amount of urobilin eliminated by the kidney (3 mg / 24 hours). Higher concentrations are indicated by a color change in the urine, which takes on a mahogany red color (hyperchromic urine) and does not form foam.
Due to the liver's key role in intestinal elimination of urobilin, an increase in urinary concentrations often, but not necessarily, reflects liver problems.
NOTE: The presence of urobilin in urine is the result of the oxidation of urobilinogen.
What's this
Urobilin is a bile pigment derived by oxidation from urobilinogen. The precursor of the latter is bilirubin, which, after being conjugated with glucuronic acid in the liver, is eliminated in the bile.
Once in the small intestine, bilirubin undergoes a reduction process becoming urobilinogen, of which:
- Some of it goes in the stool (stercobilinogen);
- Part of it is reabsorbed by the intestinal mucosa, returns to the circulation and is returned to the liver. From there, urobilinogen can be released into the bile or reach the kidney to be oxidized to urobilin and excreted in the urine.
If the amount of urobilin increases above the values considered normal, it is possible the presence of dysfunction of the liver (viral, acute and chronic, toxic liver diseases, cirrhosis, neoplasms) or of the gallbladder (obstruction of the biliary tract), or a haematological disorder (haemolytic anemia).
Even when urobilin values are particularly low or absent, abnormalities in liver function, with cholestasis or obstructive jaundice, are likely.
Urobilina: biological significance
- Bilirubin derives from the degradation of hemoglobin, a protein present in red blood cells with the task of transporting oxygen and transferring it to the tissues.
- Bilirubin is produced in the spleen, in an insoluble form called indirect bilirubin, then transported to the liver bound to albumin. In the liver the molecule acquires solubility in water through conjugation with two molecules of glucuronic acid (from this moment on we speak of direct or conjugated bilirubin).
- Conjugated bilirubin is water-soluble and as such is released into the bile, channeled into the biliary tract, accumulated in the gallbladder and poured into the intestine (duodenum).
- In the terminal ileum and colon direct bilirubin is transformed into urobilinogen by bacterial beta-glucuronidase, which splits it to glucuronic acid and bilirubin; the latter is further processed and converted into urobilinogen, mesobilinogen and stercobilinogen, all colorless substances.
- The urobilinogen is mostly excreted with the faeces, in the form of colored pigments (bilirubin → urobilin → stercobilin). A 20% is reabsorbed by the blood and conveyed to the liver, where it is again excreted with the bile.
- A small amount of the reabsorbed urobilinogen escapes the hepatic filter and is excreted in the urine, where it is oxidized to urobilin, a substance responsible for their characteristic color. The urobilinogen is in fact colorless, but is transformed by light and pH into red urobilin. Orange; for this reason, urine left to "age" after excretion has a darker color than fresh urine.
- Non-conjugated bilirubin is fat soluble. Therefore, if present in the blood at high levels it accumulates in the skin and in the ocular sclera, giving it yellowish tones (jaundice); in the child, moreover, it can reach the brain, causing more or less serious damage (nuclear jaundice).
Because it is measured
The test measures the concentration of urobilin in the urine.
This test allows you to evaluate liver function and helps diagnose any anemia caused by the destruction of red blood cells (haemolytic anemia). In addition, the urobilin test is useful for monitoring neonatal jaundice and checking the health of the newborns. kidneys.
Urine with excess urobilin is yellow-brown in color and does not foam.
Normal values
Under normal conditions, urobilin is not present in urine or is found only in trace amounts.
- Urobilin in urine - Normal values: absent or traces.
Urobilina Alta - Causes
The concentration of urobilin in the urine can increase for two different reasons.
The main causes of a high bile pigment are:
- Deterioration, damage or injury of liver cells (secondary to malignancy; viral, acute or chronic hepatitis; toxic hepatitis or liver cirrhosis);
- Increased destruction of red blood cells, such as in the presence of haemolytic anemia and severe contusions with hematomas in the course of resorption.
Low Urobilin - Causes
An absence of bile pigments is typically observed in complete obstructive jaundice.
A low urobilin value can also be observed in the presence of the following conditions:
- Enzyme deficiencies;
- Severe liver failure;
- Alteration of the intestinal bacterial flora;
- Prolonged intake of antibiotics.
How it is measured
The urobilin concentration is measured with a urinalysis.
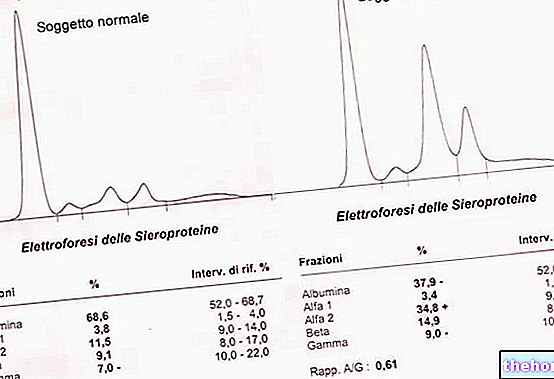
To ascertain whether the high level of this compound is due to excessive hemolysis or hepatic impairment, other tests may be performed in conjunction, such as:
- Complete blood count with red blood cell count
- Liver function test.
Preparation
For the evaluation of urobilin it is necessary to collect a small amount of urine in the morning, fasting, after having carried out an accurate intimate hygiene and after having let go of the very first emission (which may contain germs present outside the system) . In the case of women, it is good to carry out the examination away from the menstrual period.
The urine must be collected in a sterile container, which must be carefully closed immediately afterwards and taken to the laboratory within a short period of time.
Before undergoing the urinalysis useful for the evaluation of urobilin, it is good to pay attention to the type of medicines you are taking, as they can influence the result.
The doctor may find it necessary to temporarily stop taking certain medicines such as, for example, sulfonamides, phenothiazine-based drugs, acetazolamide, chlorpromazine and cascara-based anthraquinone laxatives.
Interpretation of Results
The diagnosis of the causes of an increase in urobilin is reserved to the doctor, who may also recommend other more specific tests (such as blood tests or ultrasound scans) to complete the clinical picture.
High Urobilin
The urobilin values increase in hyperemolytic states, therefore in the presence of excessive catabolism of red blood cells, typical of the so-called haemolytic anemia, or of severe contusions with hematomas in the process of resorption.
As anticipated, high levels of urobilin in the urine can indicate lesions of the liver cells (viral, acute or chronic hepatitis, toxic hepatitis, cirrhosis, neoplasms), with consequent inability to fix the bilins absorbed by the enteropathic circulation.
Low Urobilin
Low urobilin values are observed in case of:
- Complete obstructive jaundice;
- Congenital enzyme insufficiency jaundice (Crigler-Najjar syndrome, an inherited genetic syndrome in which glucuronyl transferase is lacking, physiological jaundice of the newborn and breast milk jaundice);
- Severe liver failure;
- Prolonged intake of antibiotics (on the contrary, in the presence of a bacterial hyperproliferation, as in the blind loop syndrome, an increase in urinary urobilin is appreciated).
Finally, significant variations in urinary pH can affect urobilin values: alkalinity causes an increase, greater acidity a decrease.





.jpg)


















