Definition and Causes
What is meant by High Blood Pressure in Pregnancy?
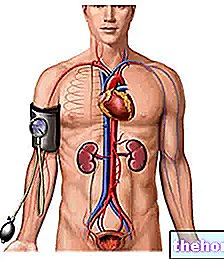
Blood pressure begins to decrease progressively after the first weeks of pregnancy, stabilizing around 75 mmHg (diastolic pressure) for the rest of the first and second trimester of gestation. In the last two - three months preceding the birth, however, the blood pressure values return to pre-pregnancy levels, therefore around 85 mmHg as regards the diastolic. We talked about minimum pressure, since the drop is mainly due to diastolic blood pressure (PAD) and - beyond the starting values - in the first and second trimester it can be quantified in about 7-10 mmHg.

A very important organ for the success of pregnancy is the placenta, which represents the communication interface between mother and fetus. At this level, in fact, thanks to an articulated system of blood vessels and microvessels, the blood of the two organisms exchange of nutrients, waste substances and gases, without direct contact between the two fluids In order for all these exchanges to take place, a considerable amount of maternal blood must reach the placental level, with reduced speed and equally low pressure.
A very important organ for the success of pregnancy is the placenta, which represents the communication interface between mother and fetus. At this level, in fact, thanks to an articulated system of blood vessels and microvessels, the blood of the two organisms exchange of nutrients, waste substances and gases, without direct contact between the two fluids In order for all these exchanges to take place, a considerable amount of maternal blood must reach the placental level, with reduced speed and equally low pressure.
When the formation of the placenta is not complete or is defective, the final product does not work as it should: its resistance, not low enough, induces an increase in pressure upstream, that is in the maternal organism. Unfortunately, during pregnancy, high blood pressure it is dangerous for maternal and fetal health, so much so that in extreme cases it can endanger the very life of both organisms. This form of hypertension, which affects about 6-8% of pregnant women, is known as gestational or induced hypertension. pregnancy. Often, high blood pressure in pregnancy is associated with urinary loss of proteins (proteinuria) and, in this case it is called gestosis or preeclampsia. Precisely for this reason, blood pressure values are carefully monitored at each obstetric check-up. during which urinalysis is always provided.
Hypertension in Pregnancy
Hypertension in pregnancy is defined as the presence of one or more of the criteria illustrated below, found in at least two measurements taken at least 4 hours apart:
- Findings of blood pressure ≥ 140/90 mmHg
- Increased (maximum) systolic blood pressure, relative to preconception, ≥ 25 mmHg (WHO) or ≥ 30 mmHg (ACOG)
- Increase in (minimum) diastolic blood pressure, relative to preconception, ≥ 15 mmHg
ACOG = American College of Obstetrics and Gynecology; WHO = World Health Organization.
Preeclampsia
Preeclampsia is characterized by the onset of hypertension (as defined above), proteinuria (> 0.3 g / 24 hours) and / or edema (feet, face, hands) after the twentieth week of gestation, in a previously normotensive woman. Preeclampsia is a wake-up call for an even more severe form of gestational hypertension, eclampsia, characterized by the onset of seizures.
Predisposing factors for preeclampsia
Nulliparity (risk> 6-8 times)
Twin pregnancy (risk> 5 times)
Diabetes
Hydatidiform mola and fetal hydrops (risk> 10 times)
Preeclampsia in previous pregnancies
Chronic hypertension
Extremes of age
Symptoms of preeclampsia
Clinical manifestations of hypertensive disorders can appear at any time during pregnancy, from the second trimester to several days after delivery. They include:
hypertension, tachycardia, changes in respiratory rate
Headache, dizziness, buzzing, drowsiness, fever, hyperreflexia, diplopia, blurred vision, sudden blindness.
Nausea, vomiting, epigastric pain, hepatomegaly, haematemesis.
Proteinuria, edema, oliguria or anuria, hematuria, hemoglobinuria.
Eclampsia
Eclampsia is defined as the presence of generalized convulsions, due to encephalopathy associated with preeclampsia and not attributable to other causes. it is a rare, but serious complication (1: 2000 births in developed countries) of hypertension gravidarum.As the name suggests, hypertension in pregnancy disappears at the end of gestation. Of course, women who have high blood pressure even before pregnancy tend to maintain their hypertension even during and after gestation. However, as anticipated in the part introductory, this magical event is accompanied by a physiological pressure drop, which requires a possible therapeutic adjustment or even the suspension of the same until the third trimester.
The greatest risks occur when a previous hypertension is added to that induced by pregnancy, the causes of which are to be found in placental hypoperfusion, reduced renal function, as well as in vasospasm and haemoconcentration.
One of the most serious clinical pictures associated with "pregnancy hypertension is the so-called HELLP syndrome, an acronym for the signs and symptoms that characterize it:
- Hemolysis (Haemolysis);
- Elevated liver enzymes;
- Reduced values of platelets (Low Platelets).
In summary, hypertension in pregnancy can be present in four distinct forms:
- Chronic pre-existing hypertension
- Gestational hypertension
- Preeclampsia / eclampsia
- Chronic hypertension + preeclampsia
Risks of Hypertension in Pregnancy
Hypertension occurs in approximately 6-8% of all pregnancies and contributes significantly to fetal growth arrest, as well as fetal and neonatal morbidity and mortality.
In Western societies, in particular, hypertension in pregnancy represents the second cause of maternal death after thromboembolism, accounting for about 15% of all causes of death in pregnancy. The pregnant hypertensive is, in fact, more predisposed to some potentially complications lethal, such as:
- The detachment of the placenta;
- Disseminated intravascular coagulation;
- L "cerebral hemorrhage;
- L "liver and kidney failure.
Treatment and Prevention of High Blood Pressure in Pregnancy
See also: Medicines for the Treatment of Gestational Hypertension
The picture that emerged from the previous paragraph is rather disturbing; however, speaking of increased risk does not necessarily mean high probability. In fact, hypertension in pregnancy can be controlled through appropriate drug therapies; however, it is essential to discover and treat the disorder early, by implementing a whole series of preventive measures.
The therapeutic choice differs in relation to the type of pregnancy hypertension and its severity. When the condition is chronic, therefore pre-existing:
- In the case of diastolic blood pressure between 90 and 99 mmHg, the treatment is essentially behavioral, therefore aimed at controlling or reducing body weight, moderation of dietary sodium, and abstention from alcohol, smoking and severe exertion. The risks for mother and fetus are quite low.
- If the diastolic pressure reaches and exceeds 100 mmHg, the treatment is pharmacological and based on the use of drugs such as alpha-methyldopa, nifedipine, clonidine or labetalol. Also in this case, the risks for the mother and fetus are low, but increase all "increase in" the extent of the hypertensive phenomenon.
PLEASE NOTE: in the mild forms, the physiological pressure drop that occurs during the first trimesters of pregnancy often gives the possibility to reduce - and sometimes suspend - the antihypertensive drugs, which will then eventually be resumed in the last two or three months of gestation.
Some medications used to treat hypertension are contraindicated in pregnancy; therefore, women of childbearing age suffering from chronic hypertension should consider the dangers associated with the use of ACE inhibitors, diuretics and sartans (to be avoided if they are trying to stay pregnant).
In the presence of pre-eclampsia, the treatment becomes more complex, so much so as to provide for a careful control of the patient, possible hospitalization with bed rest and careful monitoring of the timing of delivery. This event must be taken seriously in the face of episodes of fetal distress or a worsening of maternal conditions. Neonatal complications are mostly linked to the need to anticipate delivery at a very early time, in order to limit maternal complications.
The National High Blood Pressure Education Program recommends starting antihypertensive therapy when the minimum pressure is 100-105 mmHg or higher; the World Health Organization, on the other hand, recommends lowering blood pressure when it is around 170/110 mmHg, in order to protect the mother from the risk of stroke or eclampsia; finally, for other experts, PAD should be maintained between 90 and 100 mmHg.
Magnesium sulfate is the treatment of choice for the prevention and treatment of eclampsia.
PLEASE NOTE: women who have suffered from high blood pressure during pregnancy are exposed to a greater risk of becoming hypertensive again with the passing of age. The positivity to this test, which in some respects could be considered screening, should therefore be understood as a warning to regularly check your blood pressure (even after the end of pregnancy), and to implement all those healthy behavioral habits necessary to contain cardiovascular risk (achieving and maintaining a healthy weight, abstention from smoking and drugs, moderation of consumption alcohol, regular physical activity, optimal management of daily stress and balanced diet).