Pregnancy is a period punctuated by intense and evident changes in the female organism, supported in large part by hormonal changes that begin even before conception. Let us briefly recall how from the moment of ovulation - which occurs roughly in the middle of each menstrual cycle - i progesterone levels begin to rise in order to prepare the uterus for pregnancy.
Main functions of progesterone:
- contributes to the development of the product of conception even before it is implanted, specifically enhancing the tubal and uterine secretions necessary for the nourishment and development of morula and blastocysts (aggregates of cells that form in the first stages of embryogenesis after fertilization);
- prepares a uterine environment suitable for a possible implant;
- it induces the development of decidual cells in the endometrium, important for the nutrition of the embryo in the early stages;
- it inhibits the contractility of the pregnancy uterus, avoiding the possibility of a spontaneous abortion;
- prepares the mammary gland for lactation by promoting tubulo-alveolar development.
A few days after conception, the levels of human chorionic gonadotropin, a hormone produced by the trophoblast and the placenta that derive from it, also begin to increase. Human chorionic gonadotropin keeps the corpus luteum formed following ovulation active; in this way the levels of progesterone and estrogen continue to increase, also thanks to the gradually increasing contribution of the placenta. Thus, starting from the third month of pregnancy, the human chorionic gonadotropin levels tend to decrease quite noticeably, stabilizing around the twentieth week.

Estrogen and progesterone constantly increase during pregnancy to conserve the endometrium, prepare the mammary gland for lactation and suppress the development of new ovarian follicles. In the first trimester of pregnancy, the origin of stereoid hormones is mainly represented by the corpus luteum, thanks to support human chorionic gonodotropin; in the second and third trimesters, it is the placenta that performs this function.
Main functions of human chorionic gonadotropin (HCG).
It stimulates the corpus luteum to secrete even higher quantities of its hormones, such as estrogen and especially progesterone, avoiding its regression. These hormones, as anticipated, ensure that the endometrium (the innermost lining of the uterus) continues to develop and store large quantities of nutritional material, protecting it from the flaking experienced by every woman at the time of menstruation.
Thanks to the stimulation of the growth and hormonal secretion of the corpus luteum, human chorionic gonadotropin maintains the decidual characteristics of the endometrium, necessary for the first stages of development of the placenta and other tissues of the fetus.
Gonadotropin is used as an index to ascertain pregnancy and its correct development in the first few weeks.
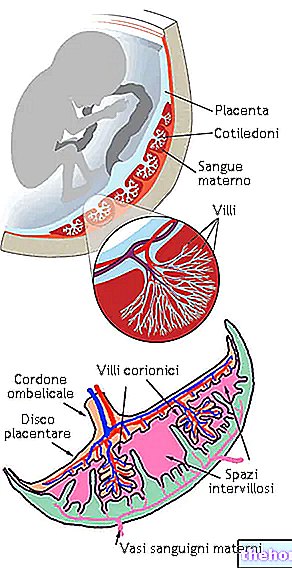
The placenta begins to form already in the very early stages of embryogenesis, to assume a definitive structure around the third month and continue to grow until the end of pregnancy. Its marked endocrine function is mainly aimed at the synthesis of chorionic gonadotropin, estrogen and progesterone.
Similarly to what has been seen for progesterone, estrogen is secreted both by the corpus luteum, in the very early stages of pregnancy, and by the placenta in the later stages. Unlike those of ovarian origin (where estradiol prevails), placental estrogens are led by "estriol, which exhibits a much lower" estrogenic activity (compensated, to tell the truth, by the conspicuous secretion).
Main functions of estrogen hormones
- They favor the enlargement of the uterus and breasts.
- They stimulate the development of the mammary glands and promote the secretion of pituitary prolactin.
They favor the enlargement of the external genitalia of the woman. - The high levels of estrogen and progesterone suppress the development of other ovarian follicles.
- In synergy with placental relaxin, they induce relaxation of the pelvic ligaments in order to make the sacroiliac joints and the pubic symphysis more elastic in view of childbirth. They also have a clear tendency to enhance uterine contractility, which up to a few weeks before birth is compensated by the proportional increase in progesterone.
- They actively participate in the development of the fetus.
Also worth mentioning is oxytocin, a hormone secreted by the neurohypophysis that causes the uterus to contract at the time of delivery. During labor, oxytocin is subject to one of the few appreciable positive feedback mechanisms in our body, since stimulation and stretching of the cervix induces a further release of oxytocin.
After delivery, with the expulsion of the placenta, hormone concentrations return to basal levels, except for the prolactin values which remain elevated; as the name suggests, this hormone is of crucial importance for lactation (inhibited during pregnancy from estrogen and progesterone). After delivery the secretion of milk is stimulated by sucking, which promotes both the release of prolactin and oxytocin (this hormone stimulates the ejection of milk). During pregnancy another hormone - called chorionic somatomammotropin human or placental lactogenic hormone - contributes to the preparation of the mammary gland for the subsequent milk secretion, mimicking the biological action of prolactin.














.jpg)











