Generality
The term heart attack it refers to the death (necrosis) of a more or less extensive part of an organ, resulting from a severe lack of blood flow. We can therefore have heart attacks (the most common), but also intestinal, cerebral, pulmonary, etc.

Causes
For further information: Intestinal Infarction - Causes and Symptoms
There are numerous causes that can lead to suffering and death of the intestinal tissues due to a deficit of local blood flow:
- occlusive causes of arterial origin: total or partial obstruction of an artery (arterial embolism and thrombosis, the former often resulting from septic endocarditis or atrial fibrillation, the latter from atherosclerosis);
- occlusive causes of venous origin: partial or total occlusion of a vein (venous thrombosis), portal hypertension, abdominal inflammation (pancreatitis, diverticulitis, appendicitis, pelvic abscess ...), paraneoplastic conditions;
- non-occlusive causes: heart failure (the heart cannot pump enough blood to meet the demands of the tissues, so intestinal infarction can also be the result of a previous heart attack), severe hypotension, local infections, excessive blood viscosity (blood difficult to circulate because they are too dense), severe spasm of blood vessels (which contract excessively reducing the amount of blood that flows inside them; it can happen in case of strong emotional stress, abuse of some drugs such as cocaine and amphetamines or injection of high doses of vasoconstrictor drugs)
- combination of two or more of the above causes
The severity of the ischemia, therefore of the heart attack, depends on the caliber of the blocked vessel, on the development or not of collateral circulation and on the extension of the intestinal tract involved; for example, arterial embolisms are more dangerous than thrombosis, since the latter evolve more slowly giving time for the formation of collateral circles.
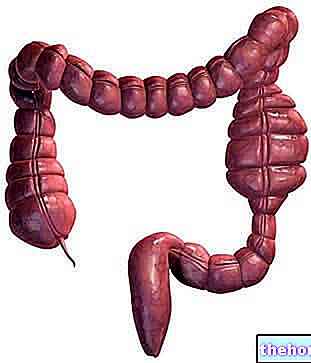
Please note: the blood vessels that supply the intestine are called mensenteric vessels (mesenteric arteries and veins); for this reason, intestinal infarction is also known as mesenteric infarction. The superior mesenteric artery (AMS) is generally involved, so the organ mainly involved is the small intestine (the right colon can also be affected); depending on the severity, the involvement of the small intestine can be total or partial (a single tract or several tracts, even discontinuous), with or without involvement of the right colon. Colon ischemia (ischemic colitis) with colonic intestinal infarction is much less frequent; in these cases the inferior mesenteric artery is involved.
Symptoms
See also: Abdominal Angina Symptoms
The symptoms of a heart attack are different depending on the organ affected, but acute pain (albeit with different localization) is almost always present. Those affected by intestinal infarction therefore complain of violent abdominal pain, but also vomiting, sometimes bloody diarrhea and In addition to this acute manifestation, typical of embolic infarcts, sub-acute pictures - generally of thrombotic aetiology - with a progressive course are also possible (the symptoms are initially more attenuated and worsen over time).
Warning symptoms of mesenteric ischemia with possible evolution into intestinal infarction, include malabsorption syndromes and angina abdominis (abdominal pain associated with digestion) with weight loss.
Diagnosis
Early diagnosis is very important but difficult, due to sub-acute symptoms, often vague without specific clinical signs, late hospitalization and reduced availability of reliable diagnostic procedures in emergencies.
Intestinal infarction is clearly evident through radiological examinations such as CT and arteriography.
Treatment
While many patients survive myocardial infarction, sometimes without realizing it (silent infarction), in the absence of treatment, intestinal infarction progresses towards death (peritonitis and sepsis) in almost 100% of cases. It is therefore an emergency condition to be dealt with promptly through adequate treatment.
- If caused by a vascular occlusion and addressed early (within 6-8 hours), the intestinal infarction can be overcome by administering thrombolytic and anticoagulant drugs.
- If caused by insufficient blood supply due to heart failure, severe hypotension, excessive blood viscosity etc. doctors intervene with adequate emergency treatments to restore an adequate blood volume and blood pressure tone.
- It should be borne in mind that the sudden reperfusion after a long ischemic period leads to the release into the circulation of free radicals deriving from anaerobic metabolism, which can lead to cardiac arrest and / or multi-organ failure; this phenomenon is known as reperfusion shock
If the diagnosis is late, intestinal necrosis requires immediate surgical treatment to avoid the extension of lethal infectious phenomena; during the operation, doctors will remove the necrotic segments of intestine and restore sufficient blood circulation (embolectomy: removal of the embolus; thromboendarterectomy: removal of the thrombus from the artery and its endothelial tissue; possible aortic-mesenteric bypass: bypassing the obstruction grafting a segment of the vessel between the aorta and the tract downstream of the obstruction).
The prognosis depends on numerous factors: time elapsed from intestinal infarction to successful treatment, extent of necrosis and surgical resection, underlying causes of the heart attack and general condition of the patient (age, concomitant diseases, etc.)