What is Conization?
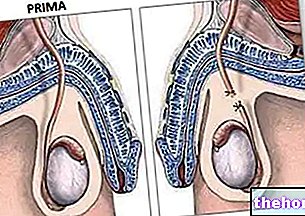
Conization is a minor surgery, generally performed on an outpatient basis with the aim of removing the lesions of the cervix highlighted during colposcopy and cervical biopsy. More specifically, the conization operation removes a small part of the cervix , generally cone-shaped (hence the term conization), comprising the cervical canal for a variable part of its height.

Conization surgery generally preserves the woman's possibility of having children, although it can increase the risk of incompetent cervix, therefore of premature birth in the event of subsequent pregnancies.
How it is done
Conization can be performed with different techniques under colposcopic guidance, each with its advantages and disadvantages; Beyond what has been expressed, it is obviously up to the doctor to describe the individual methods to the patient and the reasons that lead him to prefer one rather than another:
- conization with cold blade scalpel → traditional surgical excision, requires hospitalization and general or less frequently local anesthesia → increases bleeding risks compared to other techniques, but provides better histological samples → this technique has limited use today, for example for lesions of glandular origin (which go deeper)
- conization with diathermic loop → conization is called LEEP (Loop Electro Escission Procedure) or LLETZ (large loop excision transformation zone) → tissue removal occurs by cutting and coagulation in the points where the electrode comes into contact with the tissue. This involves minimal thermal damage on the edges of the cut, therefore the reading of the histological preparation it is not hindered → low bleeding risk, low costs
- conization with CO2 laser → takes the name of laserconization → can be performed both outpatient and day surgery under local anesthesia → allows the respect of healthy tissue but can sometimes injure the histological sample, moreover it has high operating costs
The removal of the cervical tissue cone allows to perform the histological examination, providing the pathologist with useful information on the nature and extent of the lesions. In addition to representing an "important therapeutic technique, therefore, conization can also be defined as a diagnostic technique. while the "conservative" adjective emphasizes the ability NOT to substantially alter the architecture and physiology of the uterus.
Due to its characteristics, conization is defined as an "excisional" treatment. In this sense it differs from other surgical techniques classified as "destructive": in the latter case the abnormal area, visualized by the colposcopy, is eliminated with techniques that exploit cold or heat, such as for example DiaTermo-Coagulation (DTC ), cryotherapy or laser-vaporization. Such techniques DO NOT allow to perform the histological examination of the tissue, as this is destroyed: hence the "destructive" attribute.
When is it indicated?
The destructive techniques listed above are generally reserved for cases of mild dysplasia (CIN 1 or LSIL) or in any case limited to the exocervix, while moderate or severe dysplasia cases (CIN II, CIN III or HSIL) and carcinoma in situ must be addressed with ablative, generally resolutive (therapeutic conization).
Excisional surgery can also include recourse to hysterectomy, and therefore to surgical removal of the uterus in its entirety, indicated in the case of carcinoma that is already invasive (in this case, the conization is very likely not a definitive treatment). In addition to the severity of the lesion, the choice between conization and hysterectomy is made on the basis of age, the woman's desire for future pregnancies and the history of relapses after conservative treatments.
Risks and complications
Conization is a simple and safe but at the same time delicate procedure. Generally performed under local anesthesia, it can cause discomfort or mild pain when the anesthetic is injected into the cervix. In most cases, the intervention has a short duration, about 10-20 minutes, and the woman can return home immediately; other times the intervention is longer and requires hospitalization for 24 hours.
In exceptional cases, complications can arise such as:
- bleeding during surgery
- post-surgery haemorrhage (after 2-3 weeks, at the time of the fall of the so-called escarra from diathermocoagulation or the detachment of the haemostatic points → not to be confused with the normal presence of blood losses of varying duration in the days after surgery)
- cervical stenosis with fluid retention in the uterus cavity
- infections and inflammations
- injuries of the bladder or rectum
- uterine perforation
The complete healing of the uterine neck usually occurs in a few weeks after the operation. The pain present in the following days can possibly be controlled by the use of pain relievers.
Heavy exercise should be avoided in the first few days, while no contraindication exists for normal work, study and school activities.
After 3-6 weeks, normal sex life can be resumed and vaginal tampons can be used.
Results
In most cases (> 90%, up to 97%), conization is an adequate and decisive therapy, regardless of the technique used. In spite of this, it is advisable not to let your guard down: careful monitoring of the patient after the operation is essential to prevent and identify any recurrence.